Erythropoiesis, Hemopoiesis, Hemoglobin and Roles of red cells in oxygen transport
Hemopoiesis (hematopoiesis) is the formation of balanced amounts of different blood elements. The number of daily formed blood elements must equalize the amount of daily destroyed elements. Hemoppoiesis includes erythropoiesis, thrombopoiesis, granulopoiesis, monopoiesis, and lymphopoiesis.
Erythropoiesis
It is the formation of RBCs, The whole process for the production of mature RBCs takes about 7 days. Erythropoiesis involves the following stages:
- PHSCs.
- MHSCs.
- Colony forming unit-erythrocytes (CFU-E).
- Proerythroblasts: they are the first recognizable erythrocyte precursor. They are large cells with basophilic cytoplasm.
- Basophilic erythroblasts: at this stage hemoglobin synthesis is most active. The cytoplasm is strongly basophilic due to abundant polysomes.
- Polychromatophilic erythroblasts: hemoglobin is accumulating in large quantities in the cytoplasm, ribosomes are still abundant. Accordingly, the cytoplasm shows eosinophilic areas alternating with basophilic spots. These cells represent the last stage in which the cells undergo repeated cell divisions. The coming phases involve the morphological maturation of the erythroblasts.
- Orthochromatophilic erythroblasts (normoblasts): the synthesis of hemoglobin is completed and ribosomes are much reduced in number. The nucleus becomes small and condensed. It is gradually pushed towards the periphery, extruded from the cell to be phagocytosed by the bone marrow macrophages.
- Reticulocytes: they are non-nucleated immature RBCs. They differ from mature RBCs in that: They are slightly larger. Their cytoplasm contains remnants of ribosomes and other organelles which, on staining with cresyl blue stain, form a reticulate pattern. They represent about 1% of all RBCs in a normal blood film. An increase in this percentage indicates an accelerated rate of erythropoiesis. to compensate for anemia or hemorrhage.
- Mature RBCs.
Roles of red cells in oxygen transport
Red blood cells (erythrocytes) transport hemoglobin, which is the main carrier of O2 in the circulation. In normal adults, the red cells occupy about 45% of the volume of the blood, this percentage volume of red cells in relation to whole blood is the hematocrit value.
Combination of hemoglobin with oxygen
The most important feature of hemoglobin is its ability to combine loosely and reversibly with O2. Hemoglobin binds O2 to form oxyhemoglobin, O2 is attached to the Fe2+ (ferrous iron) in the heme. The affinity of hemoglobin for O2 is affected by changes in pH, temperature, and concentration of certain substances in the red cells.
If blood is exposed to various drugs and other oxidizing agents, the Fe2+ in the hemoglobin molecule is converted to ferric iron (Fe3+) forming methemoglobin which is uncapable of carrying O2. Carbon monoxide reacts with hemoglobin to form carbon monoxyhemoglobin. Hemoglobin affinity for O2 is much lower than its affinity for CO, thus reducing the O2-Carrying capacity of the blood.
Factors affecting the formation of red blood cells (erythropoiesis)
The formation or regeneration of red blood cells is controlled by several factors that are essential for perfect red blood cell regeneration or erythropoiesis.
Tissue oxygenation role of erythropoietin
Any condition that causes the quantity of O2 transported to the tissues to decrease ordinarily increases the rate of red cell formation. The principal factor that stimulates red blood cell production is a circulating glycoprotein hormone called erythropoietin. Lack of O2 (hypoxia) stimulates the formation of erythropoietin. Most of the erythropoietin (90%) is formed in the kidney, the rest is formed mainly in the liver. Erythropoietin, in turn, enhances red blood cell production by the bone marrow until the hypoxia is relieved.
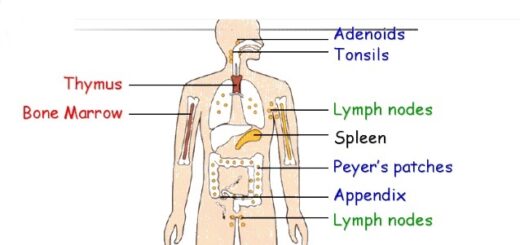
Erythropoietin stimulates the production of proerythoblasts from haemopoietic stem cells in the bone marrow. In the absence of erythropoietin, few red blood cells are formed by the bone marrow. On the other hand, when O2 transport to tissues rises above normal, the rate of erythropoietin formation decreases (negative feedback mechanism).
Nutritional factors
The cells of the bone marrow are among the most rapidly growing and reproducing cells of the body, thus they are greatly affected by the person’s nutritional status. Especially important for the formation and maturation of red blood cells are proteins, iron, vitamins, copper, and cobalt.
- Proteins: Animal proteins that are present in the liver, kidney, and muscles are superior in the production of hemoglobin (globin fraction) compared to plant-derived proteins. Animal proteins contain the essential amino acids, which are neither stored nor formed in the body.
- Iron: Seventy percent of the iron in the body is in hemoglobin (heme fraction), 3% in myoglobin, and the rest is mostly in ferritin, which is present in enterocytes, hepatocytes, and many other cells. Iron is also a constituent of cytochrome enzymes needed for intracellular oxidation.
- Vitamins: The two vitamins, vitamin B12, and folic acid are required for formation of thymidine triphosphate, an essential building block of DNA. Thus they are important for nuclear maturation and cell division of red cell precursors and are called maturation factors. The other vitamins (including vitamin C) influence the general metabolism and growth of body tissues including the bone marrow, they are not specific for red blood cell formation.
- Copper and Cobalt: Copper and Cobalt act as catalysts in hemoglobin synthesis.
Hormones
Hormones are required for erythropoiesis as they promote tissue metabolism in general. However, they are not specific except erythropoietin. Thyroxine hormones are the most powerful stimulant of body metabolism and their deficiency for a long time can cause anemia. Male hormones (androgens) and growth hormones stimulate body metabolism and erythropoiesis.
Liver
A healthy liver is essential for normal red blood cell formation. The liver manufactures globin, stores iron, copper, vitamin B12 and folic acid, and a small fraction of erythropoietin.
Bone marrow
It is the factory in which red cells and most other blood cells are formed. Destruction of bone marrow by irradiation, chemicals, drugs, or bacterial toxins will lead to the deficiency of all blood cells which is called aplastic anemia.
Blood constituents & Physical properties, Sources & functions of plasma proteins
Red blood cells (Erythrocytes) structure & function, Myeloid tissue & Bone marrow
Hemoglobin structure, review & Types of normal hemoglobin
Abnormal types of hemoglobin, Sickling of RBCs, Types & causes of methemoglobinemia
Heme biosynthesis & Disorder, Types of porphyrias, Fate of RBs & Catabolism of Hemoglobin












Hello, I am a caregiver to and advocate for a porphyria patient. This information has been very helpful
Thank you for your comment
Hi, very helpful, Thanks!
You are welcome