Endocrine system structure, function, disorders, Endocrine Glands and Hormones types
Endocrine system
The endocrine system and the nervous system are the two main coordinating and integrating systems of the body. The two systems are linked, however, through the hypothalamus which controls the secretion of many of the endocrine glands.
Endocrine glands, in general, are composed of a group of secretory cells of epithelial origin supported by a highly vascular connective tissue. The secretory cells discharge their hormones in the interstitial spaces from which they are rapidly absorbed into the circulatory system via fenestrated capillaries to reach the target organs and cells.
Histologically the endocrine system consists of:
- Individual endocrine glands e.g. the pituitary gland, the thyroid gland, the parathyroid gland, the suprarenals, and the pineal body.
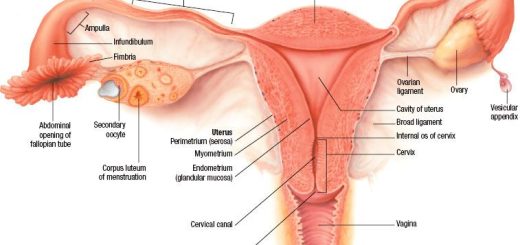
- Group of endocrine cells in certain organs e.g. pancreas (islets of Langerhans), testis (interstitial cells of Leydig), ovary (ovarian follicles and corpus luteum), placenta.
- Dispersed endocrine cells e.g. APUD cells.
Hormones
Types of hormones
- Endocrine hormones: They are synthesized by endocrine glands and transported by the blood to their target cells, e.g. Catecholamines and insulin.
- Paracrine hormones: They are synthesized near their targets of action, i.e. cell to cell action, e.g. a and β-cells of the pancreas.
- Autocrine hormones: They exert their actions on the cells of their own synthesis, e.g. Prostaglandin.
The Principal Endocrine Glands are:
- Pituitary gland (anterior & posterior).
- Thyroid gland.
- Parathyroid glands.
- Adrenal or supra renal gland (cortex & medulla).
- Islets of Langerhans (in the pancreas).
- Male gonads (testes) & female gonads (ovaries).
- Placenta.
Other Endocrine Organs
- The kidneys: The kidneys secrete: Renin, Erythropoietin, 1.25dihydroxycholecalciferol, and Certain prostaglandins.
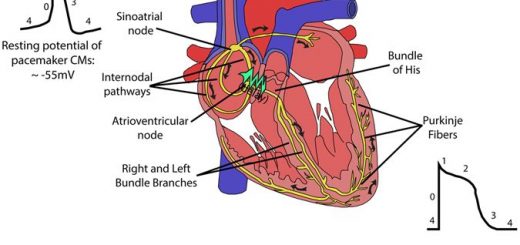
- The heart: Its atria secrete the ANP (atrial natriuretic peptide) which causes natriuretic and hypotensive effects.
- Adipose tissue: It secretes a number of hormones known as adipokines such as leptin, adiponectin, and resistin.
Chemistry of Hormones and General structure of cells secreting it:
1- Steroid hormones
- The adrenal cortex “cortisol & aldosterone”.
- The ovaries “estrogen and progesterone”.
- The testes “testosterone”.
- The placenta “estrogen and progesterone”.
General structure of cells secreting steroid and fatty acid derivatives:
- Eosinophilic and vacuolated cytoplasm.
- Well-developed smooth endoplasmic reticulum.
- Mitochondria with tubular cristae.
- Lipid droplets.
2- Derivatives of the amino acid tyrosine
- Thyroid hormones (Thyroxine & triiodothyronine) are iodinated forms of tyrosine derivatives.
- Adrenal medullary hormones (catecholamine) are derived from tyrosine.
3- Proteins or Peptides
General structure of cells secreting protein hormones, polypeptides, and amino acids derivatives
- Euchromatic nucleus with a prominent nucleolus.
- Basophilic cytoplasm.
- Well-developed rough endoplasmic reticulum.
- Well-developed Golgi apparatus.
- Mitochondria with lamellar cristae.
- Secretory granules.
Hormone Transport and Inactivation
Hormone Receptors and Their Activation:
- In the membrane: for the protein, peptide & catecholamine hormones.
- In the cytoplasm; for the different steroid hormones.
- In the nucleus; for the metabolic thyroid hormones.
Classification of hormones
- Chemical composition.
- Solubility properties.
- Site of the receptor.
- Nature of signal transmitted by them.
Hormones of group I
Hormones of Group II
- Group Ila: Includes hormones that use cAMP as 2nd messenger, e.g. epinephrine and glucagon.
- Group Ilb: Use cGMP as secondary messenger e.g. Atrial Natnuretic peptide and nitric oxide (NO).
- Group llc: Use calcium or phosphatidyl inositol or both as a second messenger e.g. vasopressin and α-adrenergic catecholamines.
- Group Ild: The secondary messenger is tyrosine kinase phosphorylation cascade e.g. Insulin.
Hormones of groups I and II
Group I
- Types: Steroids, T3, T4, Calcitriol
-
Solubility: Lipophilic
-
Carrier protein: Present
-
Plasma life span: Long (hours-days)Receptor: IntracellularMediator: Receptor-Hormone Complex
Group II
- Types: Polypeptides, proteins, catecholamines
-
Solubility: Hydrophilic
-
Carrier protein: Absent
-
Plasma life span: Short (minutes)
-
Receptor: Plasma membrane
-
Mediator: cAMP, Ca+, Phosphatidyl inositol or others
Hormonal interactions: permissiveness, synergism, and antagonism
A given hormone‘s effects are influenced not only by the concentration of the hormone itself but also by the concentrations of other hormones that interact with it. Because hormones are widely distributed through the blood, target cells may be exposed simultaneously to many different hormones, giving rise to multiple hormonal interactions on target cells. A hormone can influence the activity of another hormone at a certain target cell in one of three ways: permissiveness, synergism, and antagonism.
With permissiveness, one hormone must be present in adequate amounts for the full exertion of another hormone‘s effect (the first hormone, by enhancing a target cell’s responsiveness to another hormone, “permits this other hormone to exert its full effect). For example, thyroid hormone increases the number of receptors for epinephrine in epinephrine’s target cells, increasing the effectiveness of epinephrine. In the absence of thyroid hormone, epinephrine is only marginally effective.
Synergism occurs when the actions of several hormones are complementary and their combined effect is greater than the sum of their separate effects. An example is the synergistic action of follicle-stimulating hormone and testosterone both of which are required for maintaining the normal rate of sperm production. Synergism results from each hormone‘s influence on the number or affinity of receptors for the other hormone.
Antagonism occurs when one hormone causes the loss of another hormone’s receptors, reducing the effectiveness of the second hormone. An example of antagonistic action is the action of cortisol against the action of insulin on carbohydrate metabolism.
Endocrine disorders
Endocrine disorders commonly result from abnormal plasma concentrations of a hormone due to inappropriate rates of secretion, either too little hormone secreted (hyposecretion) or too much hormone secreted (hypersecretion) Endocrine disorder, however, may arises because target-cell responsiveness to the hormone is abnormally low, even with the normal plasma level of the hormone.
Hypersecretion, hypersecretion by a certain endocrine gland is either primary or secondary depending on whether the defect lies in that gland (as tumor) or results from excessive stimulation of the gland from the outside (as increase secretion of stimulating hormone for such gland).
Hyposecretion: hyposecretion could be also primary or secondary. Primary hyposecretion occurs when the endocrine gland is secreting too little of its hormone because of an abnormality within that gland while secondary hyposecretion occurs when the endocrine gland is (normal) but is secreting too little hormone because of a deficiency of its tropic (stimulating) hormone.
Pituitary gland function, structure, location, hormones and anatomy
Anterior pituitary gland function, hormones, location and Effects of Growth Hormone
Posterior pituitary gland hormones and function, Control of ADH and Oxytocin hormone
Endocrine system, Endocrine glands, Pituitary gland and Hormonal coordination in living organisms
Regulation of Growth Hormone Secretion and Effects of Deficiency of Anterior Pituitary Hormones
Thyroid gland, Diseases of thyroid gland and Function of Parathyroid glands