Lipoproteins, Metabolism of chylomicrons, plasma cholesterol, Lipotropic factors and fatty liver
Lipoproteins made up of droplets of fats surrounded by a single layer of phospholipid molecules, Phospholipids are molecules of fats that are attached to the phosphorus-containing group, Lipoproteins transport hydrophobic lipid molecules in water, such as in the blood plasma or other extracellular fluids, lipoproteins such as many enzymes, transporters, structural proteins, antigens, adhesins, and toxins, Examples include plasma lipoprotein particles (HDL, LDL, IDL, VLDL, and chylomicrons).
Blood lipids
Plasma lipids are usually measured after 12 hours of fasting. The total plasma lipide ranges from 400-700 mg/dl (mean value 470 mg/dl). Also include small amounts of other steroids and fat-soluble vitamins
Plasma lipoproteins
All lipids in plasma are transported in the form of lipoproteins. Plasma lipoproteins have the central core formed of non-polar lipids (triacylglycerols and esterified cholesterol). The outer layer contains the more polar lipids (phospholipids and non-esterified cholesterol), and proteins (apoproteins). Apoproteins are either peripheral (can be transferred) or integral (cannot be transferred).
Functions of apolipoproteins
- Solubilizing lipids in an aqueous environment.
- Recognition sites for receptors e.g. LDL-receptors.
- Activators for certain enzymes involved in lipoprotein metabolism e.g. apo-CIl activates lipoprotein lipase and apo-Al activates LCAT.
Types of apoproteins
- Apolipoprotein-A: These include apo-Al and apo-All. They are the major apoproteins of HDL, and they are mainly synthesized in the intestine. Apo-Al in HDL is an activator of the plasma enzyme lecithin-cholesterol acyl transferase (LCAT) which is the enzyme responsible for the formation of most of the plasma cholesteryl ester in humans.
- Apoprotein-B: It is of two types: apo-B48 for chylomicrons and it is synthesized in the intestine, and apo-B100 for LDL and VLDL, synthesized in the liver.
- Apoprotein-C: These include apo-CI, apo-Cll, and apo-CIll, synthesized in the liver and freely. transferable between several different lipoproteins. Apo-Cll is actually transferred from HDL to chylomicrons and VLDL and is an activator of plasma lipoprotein lipase.
- Apoprotein E: Apo E is found in VLDL, HDL, chylomicrons, and chylomicron remnants; it accounts for 5-10% of total VLDL apolipoproteins in normal subjects.
Metabolism of chylomicrons
I- Synthesis of nascent chylomicrons:
- Nascent chylomicrons are formed in the intestinal mucosa and pass to the chyle and then to the bloodstream through the thoracic duct.
- Triglycerides are the predominant lipid in chylomicrons and form 90% of the total lipid present in them. (Exogenous triglycerides).
- Its protein content is about 1%.
- Apo-A and apo-B48 are components of the chylomicrons, they are also formed in the intestinal mucosa
Il- conversion of nascent chylomicrons to mature chylomicrons:
After entering the bloodstream, the chylomicron particles transfer apo-A to HDL and acquire apo-C from HDL.
III- Degradation of chylomicrons:
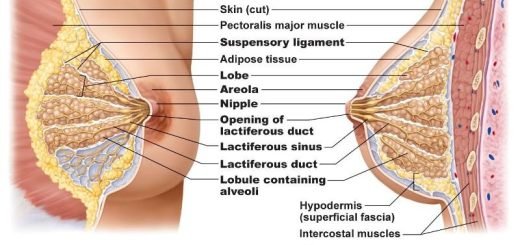
- Apo-Cll activates lipoprotein lipase (LPL= clearing factor), located in the capillaries of adipose and other peripheral tissues as cardiac and skeletal muscles and lactating mammary gland. Insulin enhances the synthesis of this enzyme and heparin increases its activity.
- Triglycerides in chylomicrons are hydrolyzed into glycerol and FFA. The fatty acids are released and oxidized in muscles or stored as triglycerides in adipose tissue. They are transported bound to plasma albumin. Glycerol is taken by the liver cells mainly due to the high activity of glycerol kinase.
IV- Formation of chylomicron remnants:
- As triglycerides are removed from the hydrophobic core of chylomicrons, the surface area of chylomicrons decreases.
- The more hydrophilic surface components (apo-C, unesterified cholesterol, and phospholipids) are transferred to HDL. The remaining particles are termed chylomicron remnants.
V- Fate of chylomicron remnants:
- They are triglycerides-poor particles and consist mainly of cholesterol esters and apo-B48.
- They interact with receptors on liver cells and are taken by endocytosis, where they are catabolized within the hepatic lysosomes and the products (amino acids, fatty acids, cholesterol) are released into the cytosol and reutilized by the hepatic cells.
Metabolism of very-low-density lipoproteins (VLDL)
I- Synthesis of nascent VLDL:
- VLDL is synthesized in the liver, particularly after a high carbohydrate meal.
- VLDL are moderately large particles.
- The triglycerides are the main lipid component (Endogenous triglycerides).
- It contains a specific apoportein 100.
II- Conversion to mature VLDL:
They are released into the blood by the liver. They receive apo-C11, E2, and cholesterol esters from HDL in plasma.
III- Degradation by plasma LPL:
- In peripheral tissues, particularly adipose tissue and muscles, VLDL triglycerides are hydrolyzed by lipoprotein lipase attached to capillary walls, into glycerol and FFA.
- The surface components of VLDL which are mainly apo-C, cholesterol, and phospholipids are transferred to HDL.
IV- Formation of VLDL remnants:
VLDL particles become smaller and are now known as VLDL remnants or LDL.
Low-density lipoproteins (LDL)
All LDL arises normally from VLDL metabolism. LDL particles are rich in cholesterol esters, which are probably derived from HDL. Apo-B100 is the only apolipoprotein in LDL particles.
Fate of LDL
LDL particles bind to specific apo-B100 receptors in both extrahepatic tissues (30%) and the liver (70%). The receptor LDL complex is internalized by endocytosis. These vesicles fuse with lysosomes where cholesterol esters are hydrolyzed by lysosomal acid lipase to free cholesterol that performs its function according to the tissue.
Cholesterol is used for.
- Biosynthesis of the cell membrane.
- Reesterified for storage inside the cell by ACAT (Acyl CoA-cholesterol Acyltransferase), which is activated by free cholesterol.
- In adrenal glands and ovaries, cholesterol is used for the synthesis of steroid hormones e.g. cortisol and estradiol. In the liver, cholesterol.
The cholesterol content of the cells that have an active LDL pathway is regulated in 2 ways:
- The released cholesterol suppresses the formation of HMG CoA reductase there by inhibiting de novo synthesis of cholesterol.
- LDL receptors are subjected to feedback regulation. New receptors are not synthesized and so the uptake of additional cholesterol from the plasma LDL is blocked.
LDL is an important source of cholesterol to extrahepatic tissues. High levels of LDL- cholesterol increase the risk of atherosclerosis.
Metabolism of high-density lipoproteins (HDL)
- These are the smallest and the most dense lipoprotein particles.
- They contain a large amount of proteins (50-60%) and very few triglycerides, while the predominant lipid is a phospholipid.
- They are formed by the liver cells and intestinal mucosa as discoidal HDL.
- They are mainly formed of a phospholipid bilayer, free cholesterol, and apo-C.
- On entering the circulation, apo-A, the major HDL apoprotein is acquired from
- chylomicrons, and apo-C is transferred to chylomicrons and VLDL.
- Apo-Al activates LCAT (lecithin – cholesterol acyl transferase) which is present on the HDL surface. Free cholesterol, present on the HDL surface is esterified by LCAT. Lecithin + Cholesterol (LCAT) → Cholesterol ester (CE) + lysolecithin
- Cholesterol esters (CE) form a central hydrophobic core that pushes the phospholipid bilayer apart and converts the discodial HDL into spherical HDL.
- More free cholesterol is transferred from the tissues (from cell membranes) or from other lipoproteins into the HDL surface.
- CE is transferred from HDL to VLDL and LDL, thus enabling HDL to perform further esterification.
So HDL is important for the removal of cholesterol from the tissues to the liver, and high levels of HDL protect against atherosclerosis.
Dynamics of plasma cholesterol:
Plasma cholesterol is in a dynamic state, entering the blood complexed with lipoproteins and leaving the blood as tissues remove cholesterol from lipoproteins or degrade them intracellularly.
High-density lipoproteins and the enzyme lecithin-cholesterol acyl transferase (LCAT) play important roles in the transport and elimination of cholesterol from the body. LCAT is a plasma enzyme produced mainly by the liver. The LCAT-HDL system functions to protect cells especially their plasma membranes from the damaging effects of excessive amounts of free cholesterol.
Cholesterol ester generated in LCAT reaction diffuse into the core of HDL particle where it is then transported from the tissues and plasma to the liver; which is the only organ capable of metabolizing and excreting cholesterol. Thus by this mechanism, reverse transport of cholesterol, LCAT acting on HDL provides a vehicle for transporting cholesterol from peripheral tissues to the liver.
Separation of lipoproteins
Plasma lipoproteins are separated into different fractions by two methods, electrophoresis, and ultracentrifugation.
1. Electrophoresis
They are separated according to their mobility in an electric field. It depends on the charge and molecular weights of various particles. According to this method, plasma lipoproteins can be separated into:
- α lipoproteins.
- β-lipoproteins.
- Pre β lipoproteins.
- Chylomicrons.
2. Ultracentrifugation
They are separated according to their density. The higher the protein content the higher the density of the particles. The main fractions separated are as follows:
- Chylomicrons.
- Very low-density lipoproteins (VLDL).
- Low-density lipoproteins (LDL).
- High-density lipoproteins (HDL).
- Free fatty acids-albumin complex. It is not considered a typical lipoprotein fraction.
Lipotropic factors
These are substances that help the mobilization of fat from the liver. They include substances essential for the biosynthesis of phospholipids and proteins, thus helping the formation of LDL, HDL, and VLDL which are necessary for the mobilization of TG from the liver. They include:
- Substances important for the biosynthesis of phospholipids: such as Essential fatty acids. Inositol, and Choline.
- Methyl donors or compounds needed for the synthesis of methyl group. Methyl group donors are needed for synthesis of choline and carnitine: Methionine. Glycine and betaine. vitamin B12 and folic acid.
- Pantothenic acid needed for the synthesis of CoA which is needed for F.A. oxidation and esterification.
- Proteins of high biological value that provide essential amino acids are important for the biosynthesis of proteins.
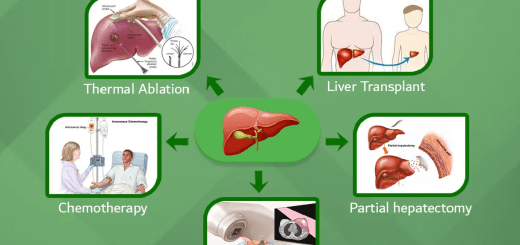
Fatty liver
It means accumulation of lipid (mainly triacylglycerols) in the liver, leading to fibrotic changes and impaired liver functions.
Causes of fatty liver
I- Causes related to lipid:
A) Causes due to excessive mobilization of fat to the liver:
- Excessive intake of lipid and carbohydrate (diet).
- Excessive mobilization of fat from adipose tissue to the liver. The plasma-free fatty acids level is increased. TG synthesis in the liver exceeds the rate of lipoprotein formation and secretion, thus the hepatic content increases. This phenomenon appears in prolonged starvation and severe uncontrolled DM.
- Alcoholism: Alcohol intake increases TG synthesis and cholesterol synthesis.
B) Causes due to decreased mobilization of fat from the liver:
- deficiency of substances called lipotropic factors which are essential for phospholipids synthesis that enter in the structure of plasma lipoproteins. Lipotropic factors are, for example, methionine, choline, ethanolamine, serine, and inositol.
- Reduced oxidation of fatty acid in the liver e.g. due to pantothenic acid and carnitine deficiency.
- deficiency of essential fatty acids or cholesterol overfeeding. Cholesterol is esterified with essential fatty acids resulting in their depletion and inhibition of phospholipids formation.
II- Causes related to protein:
- Liver poisons e.g. carbon tetrachloride that affect the conjugation of lipid to proteins to form lipoproteins or inhibit the formation of the protein part of lipoproteins.
- Protein deficiency decreased intake.
- Drugs that inhibit protein synthesis e.g. puromycin. this will lead to a deficiency in lipoproteins produced by the liver.
Lipogenesis, Synthesis of cholesterol, Fatty acid synthesis & Regulation of fatty synthesis
Capillary circulation, Regulation of vasomotion, tissue formation & Edema types & causes
Physiology of the circulatory system & How does the circulatory system work