Ankylosing Spondylitis (AS) symptoms, causes, diagnosis and treatment
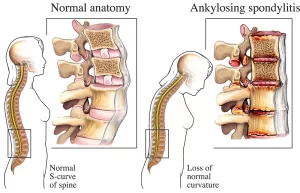
Ankylosing spondylitis causes inflammation in the joints and ligaments of the spine, It may affect peripheral joints like the knees, ankles, and hips, It is known as axial spondyloarthritis, Eye and bowel problems may occur as well as back pain, Joint mobility in the affected areas generally worsens over time.
Ankylosing Spondylitis (AS)
Ankylosing spondylitis is a chronic inflammatory disorder of unknown etiology, The disease has a striking endency towards inflammation followed by fibrosis followed by secondary ossification and total ankylosis of involved joints.
Prevalence
- Prevalence is comparable to that of RA with an increased male: female ratio (4:1). (Special disease in which male prevalence is higher than that of females).
- Women tend to have more peripheral joint manifestations thus leading to an inappropriate diagnosis of RA.
Etiology
The etiology of AS is unknown, but a combination of genetic and environmental factors may have a role in producing clinical disease.
Genetic factors:
- HLA-B27 to AS heritability is only -20%, indicating that other genetic influences contribute to AS.
- Non-HLA genes IL-23/17 A pathway confer a predisposition to AS.
Environmental factors:
- The infection could play a role as associations of active synovitis with the presence of Klebsiella species in stool, chronic prostatitis, and urethral chlamydial organisms have been reported.
- Intestinal dysbiosis (imbalance of gut microbiota) is involved in the disease onset & progression.
Pathophysiology:
The main site for the changes in AS is the enthesis (site of attachment of joint capsule, ligament and tendon into the bone) which is considered the primary site of pathology.
But it is not the only site for the pathology, there are some other sites like osteitis (subchondral bone), annular fibrosis (spine), periosteitis and synovitis (peripheral joints and ligaments).
Symptoms and Signs (Inflammatory low back pain with its criteria)
The onset is usually insidious. Intermittent bouts of back pain that may radiate down the thighs, Stiffness that is often worse in early morning hours and after prolonged rest. The pain gradually improved with exercise.
As the disease advances (3rd stage), back motion becomes limited, with (flattening of the lumbar curve and exaggeration of the thoracic curvature (Kyphosis).
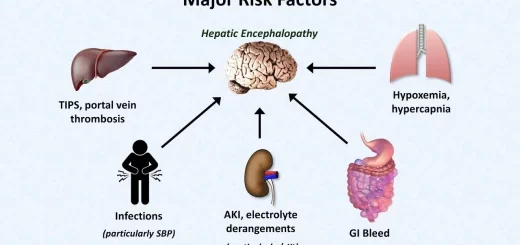
Chest affection in acute stage leads to anterior chest pain that mimics angina pectoris but in 2nd & 3rd stages (fibrosis and calcification), the pain decreased and chest expansion is often limited as consequence of costovertebral joint involvement.
Joints involved
- The axial skeleton (including sacroiliac joints, intervertebral disc spaces, and the apophyseal and costovertebral joints).
- The anterior central joints (e.g. the manubriosternal joint, sternoclavicular joint, and symphysis pubis).
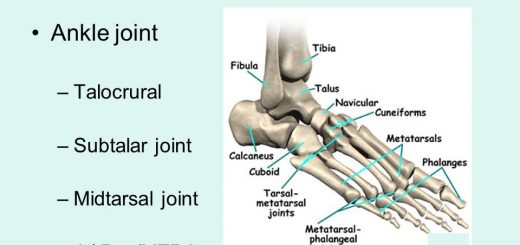
- Large proximal synovial joints in the pattern of asymmetrical oligoarticular (hip, knee, shoulders).
- Small peripheral joints are infrequently involved.
Investigations
Laboratory studies
- HLA-B27 is present in 90-95% of patients.
- The erythrocyte sedimentation rate is elevated in most cases.
- Mild normochromic normocytic anemia is seen in severe cases.
CT & MRI
They are able to detect early lesions as one of the key diagnostic tools in detecting the earliest signs of inflammation.
Forty two year old male with ankylosing spondylitis:
- Demonstrating advanced disease with bilateral subchondral sclerosis, erosions, and pseudo-widening of the sacroiliac joints.
- The entire spine demonstrating bilateral SIJ’s BME, fat metaplasia, and erosions as well as corner inflammatory lesions and fatty lesions in the spine.
Plain X-ray
X-ray could detect bony lesions in late stages.
The sacroiliac joints may show:
- Punched-out erosions.
- Pseudo-widening of the joint.
- Adjacent sclerosis with complete loss of joint space.
- Bony bridging of the joint.
The spine
- Romanus sign: shiny corners of the spine.
- Squaring of the vertebral bodies.
- Syndesmophytes: new bone formation.
- Calcification of the anterior and lateral spinal ligaments (railway appearance or bamboo Spine lateral view).
Criteria for diagnosis
Modified New York Criteria for Ankylosing Spondylitis (1984)
1. Clinical criteria:
- Low back pain and stiffness for more than 3 months which Improves with exercise, but is not relieved by rest.
- Limitation of motion of the lumbar spine in both the sagittal and frontal planes.
- Limitation of chest expansion relative to normal values correlated for age and sex.
2. Radiological criterion: Sacroilitis grade > 2 bilaterally or grade 3-4 unilaterally.
Definite ankylosing spondylitis if the radiological criterion is associated with at least 1 clinical criterion.
Prognosis
- The course of AS varies
- Spontaneous remissions and relapses are common.
- Occasionally, the disease progresses to ankylosis of the entire spine.
- Less than 10% develop crippling disease-speaking.
- In general, the functional prognosis is good unless the hips are seriously involved.
Management of ax SpA
Prior to the introduction of biologic therapies, treatment of axSpA was limited to NSAIDs and physical therapy.
Both have demonstrated efficacy in improving symptoms of inflammatory back pain and NSAIDs can also be effective in reducing the level of acute phase reactants such as C-reactive protein (CRP).
Unfortunately, axial and entheseal manifestations of SpA do not respond well to conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs).
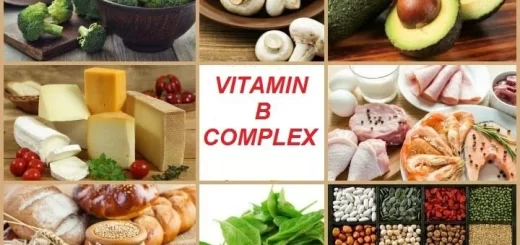
Sulfadiazine in doses reaching 1 gram twice daily is sometimes effective in relieving symptoms especially for peripheral arthritis but has little symptomatic effect on spinal and sacroiliac disease (toxicities include rash, nausea, diarrhea, and agranulocytosis), Methotrexate is of questionable benefit in AS.
- Local corticosteroid injections are useful for symptomatic sacroiliitis, peripheral enthesitis, and arthritis.
- There are currently five licensed anti-tumor necrosis factor (TNF) drugs for the indication of axSpA: Adalimumab, Certolizumab, Etanercept, Golimumab, and Infliximab.
These therapies can be used as monotherapy, without the need to combine them with csDMARDs. All, excep Infliximab with low dose of methotrexate.
The IL-17 inhibitor, Secukinumab, has also been approved by the EMA but only for axSpA patients with radiographic sacroiliitis.
Tofacitinib, (JAK) inhibitor and other drugs administered orally appear promising in clinical trials and soon will approved in AS management.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Rheumatoid Arthritis (RA) causes, stages, symptoms, diagnosis, and specific joint affection
Rheumatoid Arthritis diagnosis and treatment, Disease-Modifying antirheumatic drugs (DMARDs)