Rheumatoid Arthritis (RA) causes, stages, symptoms, diagnosis and specific joints affection
Rheumatoid arthritis is a progressive systemic chronic inflammatory autoimmune deforming disorder with unknown etiology. Rheumatoid Arthritis (RA) is characterized by joint destruction, and symmetrical swelling of joints, Causing polyarthritis in small and large Joints but mainly small joints, It is associated with systemic disturbance and extra-articular manifestations.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) typically results in warm, swollen, and painful joints, Pain and stiffness often worsen following rest, Most commonly, the wrist and hands are involved, with the same joints typically involved on both sides of the body, It is a long-term autoimmune disorder that primarily affects joints.
It may affect other parts of the body, including skin, eyes, lungs, heart, nerves, and blood, This may result in a low red blood cell count, inflammation around the lungs, and inflammation around the heart, Fever, and low energy may also be present, Often, symptoms come on gradually over weeks to months.
Epidemiology
- Prevalence worldwide: 1% worldwide, with Female/Male= 2:1.
- Prevalence in Egypt: Affects about 2% of the Egyptian population. Two out of three patients are female.
- Peak age of onset: between the ages of 45 and 65 years.
- Disability: Patients are moderately disabled within two years of diagnosis. Patients are severely disabled by 10 years.
Aetiology
Genetic background
- Association with HLA DRI, DR4, DRW14.
- Shared epitope: Increased susceptibility with a specific amino acid sequence on the B chain of HLA DR1. DR4.
- Increased in first-degree relatives.
Possible environmental factors antigens
- Virus (Parvovirus- Epstien – Barr viruses – Retroviruses).
- Bacteria (Mycoplasma – Mycobacteria).
- Smoking: (modify our self proteins and making them targets of the immune system.
Pathogenesis
- Cell-mediated Immunity through macrophage and THI lymphocytes.
- Some contribution of B lymphocytes, to Plasma cells, forming Antibodies, forming immune complexes that may be responsible for some of extra-articular features.
- Macrophages present processed antigens to THI.
The cells produce:
- IL2 stimulates lymphocytes.
- IFN stimulates macrophage.
Macrophages produce:
- IL-6: stimulates acute phase response (ESR CRP).
- IL-8 is chemotactic to polymorphs, forming: Toxic oxygen radicals, Prostaglandins, and Leukotrienes.
IL-1stimulates TNF causing:
- Activation of synovial fibroblasts and chondrocytes that form: Metallo-proteinases cause cartilage destruction, and PG-E2 leads to Demineralization and Destruction of bone.
- Upregulation of adhesion molecules with cell recruitment.
- Stimulation of angiogenesis to supply the proliferating synovium.
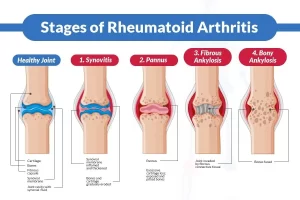
Stages of Rheumatoid Arthritis
- Healthy Joint.
- Synovitis.
- Pannus.
- Fibrous Ankylosis.
- Bony Ankylosis.
Pathology
- Early change: injury to synovial microvasculature.
- Swelling and congestion of synovial membrane and infiltration with THI lymphocytes, macrophages, and some plasma cells, leading to Effusion of synovial fluid rich in polymorphs.
- Hypertrophy of synovial membrane with villous formation. Lymphoid follicles may form.
- Formation of inflammatory granulation tissue Pannus spreading over and under the articular cartilage which becomes eroded.
- Fibrous and bony ankylosis may occur.
- Atrophy of muscles adjacent to inflamed joints.
- Inflammatory destruction of soft tissues, causing Laxity of ligaments and Tend deformities.
Clinical picture
Onset
- Gradual onset (Usually).
- Acute in a minority.
- Occasionally palindromic (Pain, Swelling, Erythema that resolve but recur. 50% develop RA).
Systemic symptoms
- Fatigue.
- Malaise.
- Weakness.
- Low-grade fever.
- Loss of weight.
Joint symptoms
Joint pain, Swelling, Tenderness on pressure, Morning stiffness due to Edema, and Inflammatory accumulation during Sleep or Inactivity.
- Commonly involved joints: Hand joints (MCP- PIP- Wrist, DIP is not involved), Foot joints, knee joint).
- Also affected joints: Shoulder, Hip, Ankle, and Sternoclavicular joints.
- Less commonly affected: Tempro-mandibular joint and cricoarytenoid joints, Spinal involvement is limited to the upper cervical area (C1-C2).
- The sacroiliac joint is spared. DIP is spared.
Specific joints affection
Hands
- The fusiform or spindle-shaped appearance of fingers due to swelling of PIP joints.
- Swan neck deformity: Hyperextension at PIP with flexion at DIP.
- Bilateral symmetrical swelling of MCP.
- Ulnar deviation of fingers at MCP joint associated with deviation at radiocarpal Joints (Zig Zag deformity of the hand).
- Boutonniere deformity: Flexion at the PIP with extension at DIP.
- Z-shaped deformity of thumb.
- MCP subluxation.
- Caput ulnae: Dorsal subluxation of ulnar styloid of the wrist, Detected by Piano key test.
- Boggy synovium at the dorsum of the wrist.
- Trigger finger: Inflamed flexor tendon sheath that prevents extension of the finger from a flexed position. A nodule formed in the tendon sheath (Locking). Muscle atrophy with weak hand grip strength.
- Thin atrophic skin due to underlying synovitis.
- Early limitation of dorsiflexion of the wrist.
- Palmar erythema and prominent veins on the dorsum of the hand indicate increased blood flow.
Feet
- Hallux valgus.
- MTP subluxation and flexion at PIP, causing Cock-up deformity of the toe (Hammer’s toe) forming Callosities.
- Fibular deviation of toes.
- Valgus deformity of ankle.
- Flattening of the longitudinal arch.
Knee
- Swelling due to synovial hypertrophy and effusion.
- Quadriceps atrophy.
- Genu valgum vs. Genu varum: “GUM” makes your knees stick together, and “RUM” makes your knees spread apart.
- Doppler ultrasound or arthrography for diagnosis. Ultrasound or MRI (Non-invasive) can now replace arthrography.
Extra-articular features (Manifestations)
- Episcleritis: It is an inflammatory condition affecting the episcleral tissue between the conjunctiva (the clear mucous membrane lining the inner eyelids and the sclera (the white part of the eye) that occurs in the absence of an infection.
- scleritis: is an inflammatory condition affecting the scleral proper.
- Scleromalacia: Painless, Bilateral Thinning. Blue color of underling choroid.
- Corneal melting: Pain, Redness, Blurred vision, Thinning, and Perforation.
- Sjogren’s syndrome: Chronic autoimmune inflammatory disease with lymphocytic infiltration and destruction of exocrine glands of eyes and mouth. Causes: Primary sicca syndrome, Secondary (to other autoimmune diseases); rheumatoid arthritis (most common).
- Pyoderma gangrenosum: It is a rare, inflammatory skin disease where painful pustules or nodules become ulcers that progressively grow. The cause is not well understood, the disease is thought to be due to immune system dysfunction and particularly improper functioning of neutrophils.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Rheumatoid Arthritis diagnosis and treatment, Disease-Modifying antirheumatic drugs (DMARDs)
Chronic Low Back Pain diagnosis, symptoms, treatment and Seronegative Spondyloarthritis types