Rheumatoid Arthritis diagnosis and treatment, Disease Modifying antirheumatic drugs (DMARDs)
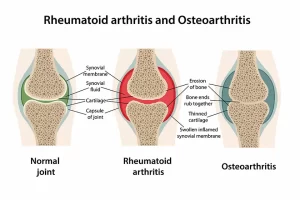
Rheumatoid arthritis causes joint inflammation and pain, It happens when the immune system doesn’t work properly and attacks the lining of the joints, called the synovium, It affects the hands, knees or ankles, and the same joint on both sides of the body, such as both hands or both knees, But sometimes Rheumatoid arthritis causes problems in the eyes, heart and circulatory system and/or the lung.
Criteria for diagnosis of RA
The ACR criteria for diagnosis of RA
- Morning stiffness at least one hour and present for at least 6 weeks.
- Swelling of 3 or more joints for at least 6 weeks.
- Swelling of wrist MCP or PIP for 6 weeks or more.
- Symmetric joint swelling.
- Hand X-ray changes: Typical changes of RA (Erosions or Unequivocal Bony Decalcification).
- Rheumatoid nodules.
- Serum RF by a method positive in less than 5% of normal.
- 4 or more criteria must be present for diagnosis.
- Criteria are not sensitive for diagnosis of early RA.
- six weeks duration of symptoms is important.
- It prevents self-limiting or viral arthritis from being labeled as RA.
Investigations and Monitoring of RA
To evaluate diagnosis:
- Clinical criteria.
- Acute phase response: ESR, CRP.
- Serological tests: Rheumatoid factor (RF).
- X-ray joints.
- Synovial fluid analysis.
To monitor disease activity and drug efficacy:
- Pain (Visual analogue scale).
- Early morning stiffness (Minutes).
- Joint tenderness (Number of inflamed joints, Articular index).
- Acute phase response.
To monitor disease damage:
- X-rays.
- Functional assessment: Health assessment questionnaire.
To monitor drug safety:
- Urine analysis.
- Biochemistry.
- Haematology.
Acute phase response:
- Elevated in widespread disease.
- May be normal in isolated small joint synovitis.
Rheumatoid factors:
- Anti-globulin antibody of class IgM. IgG, or IgA against Fe fragment of IgG.
- Agglutination tests detect IgM RF.
Latex test use polystyrene particles coated with human IgG. Rose waaler uses sheep red cells coated with rabbit anti-erythrocyte antibodies. Rose waaler is less sensitive but more specific than the latex test. RF titer has no prognostic significance. RF is positive in 85% of patients but early in 70% only.
It is also positive in:
- Sjogren’s syndrome.
- Other C.T. diseases,
- Chronic liver diseases.
- Sarcoidosis
- Multiple myeloma.
- Chronic infections: TB, Leprosy, Syphilis.
Other serological tests:
- Antikeratin antibody.
- Anticitrulline antibody.
Elisa determination of antibodies to citrullinated antigens is now used (Anti-cyclic citrullinated peptides or anti-CCP). Anti-CCP antibodies are found in:
- Early RA as well as in the preclinical phase.
- Some RF negative RA cases.
Anti-CCP are predictors of the severity of RA. Sensitivity in RA is 40% to 70%. Specificity may be 98%.
X-ray:
Early: Soft tissue swelling and Peri-articular osteoporosis.
More advanced:
- Narrowing of joint spaces.
- Marginal erosions.
- Subluxations (Mal-alignment).
- Deformities.
Synovial fluid analysis: Differentiates inflammatory arthritis (As: RA) from Degenerative as OA or septic arthritis.
In inflammatory arthritis:
- Turbid.
- WBC’s 2000-50.000%.
- Polymorph 20-70%.
- The Mucin clot is poor.
- Hyaluronic acid is degraded.
- Synovial fluid/blood glucose difference: 30.
- No crystals.
- Decreased complement.
Treatment
Early diagnosis and early treatment are needed as joint destruction occurs in the first 1-2 year onset. Aggressive treatment for patients with poor prognostic features as:
- Early onset of severe synovitis (high disease activity) with functional limitation.
- Joint erosions.
- Extra-articular manifestations.
- Rheumatoid factor positivity.
- Family history of severe RA.
Goals of therapy:
- Treat only.
- Treat to limit and/or prevent: Pain, Joint damage, Extra-articular disease, Disability, and Premature death.
- Treat to target.
Treatment includes:
- Synthetic Disease Modifying Anti-Rheumatic Drugs: Methotrexate, leflunomide, sulfasalazine, hydroxychloroquine.
- Biological agents (Anti-cytokine): Anti-TNF, anti-B cell, anti-IL-6.
- Combinations.
Physical therapy is important in:
- Passive movement to maintain full range of movement.
- Graded exercise program.
- Heat therapy: Warm pools and Paraffin bath.
- Rest splints for very painful joints.
- Surgery and Rehabilitation may be needed.
Disease Modifying antirheumatic drugs (DMARDs):
- They decrease inflammatory synovitis and prevent or retard joint erosion and destruction.
- Should be used within 12 weeks of onset, as joint damage occurs early in the disease course.
- They are used singly or in combination in severe disease.
Non-steroidal anti-inflammatory drugs (NSAIDs):
- They control inflammation and pain (Analgesic effect).
- They do not prevent the structural damage.
- Individual variation in response and toxicity.
Steroids: They have a very rapid and dramatic anti-inflammatory action, However, the doses required to maintain adequate symptomatic relief are accompanied by unacceptable side effects such as: Cushinoid features, osteoporosis, hyperglycemia, IHD, hypertension, peptic ulcers, Glucoma, Cataract.
Indications:
- Rapid, short-term (1-3 months) in control of marked synovitis while awaiting efficacy from DMARDs (Bridge therapy).
- Use a low dose (7.5 mg) of prednisolone or equivalent.
- For vasculitis, eye or lung involvement.
- During pregnancy when DMARDs are contraindicated.
Intra-articular injections:
- For temporary control of synovitis of one or a few joints.
- 2-8 weeks duration of benefit.
- Frequent injections cause joint damage (Should not be more than 4/ year in a large join).
- A strict aseptic technique is a must.
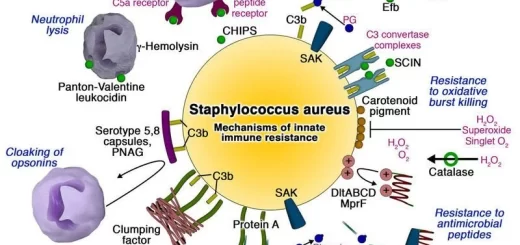
Anticytokine treatment (Biological agents):
- TNF-α antagonists:
- Anti-TNF is now available: Infliximab, Etanercept, Adalimumab, and Golimumab.
- Only Infliximab needs to be combined with methotrexate to prevent the development of antibodies to the mouse component of the drug.
Biologic Therapy: Major Safety Issues:
- Infections.
- Infusion/injection-site reactions.
- Auto-immune diseases.
- Malignancy.
- Immunogenicity, blocking antibodies.
- Use in pregnancy.
- Use in patients with congestive heart failure.
- Use in patients with cardiovascular diseases.
Treatment strategy
- Combination therapy is superior to monotherapy.
- Combination of 2 to 3 DMARD’s with (Or without) Steroids to completely control disease as early as possible.
- After 3 months: If controlled with DMARDs escalate to biologic DMARDs.
- Then taper the patient off a number of these drugs and leave him on the simplest possible long-term maintenance therapy.
- The first drug is usually Methotrexate.
- To “incomplete responders” or “suboptimal responders” or active disease despite methotrexate after 3-6 months of conventional DMARDs.
- Choices: Methotrexate in addition to one of: Leflunomide, Hydroxychloroquine, Salazopyrine, Both previous 2 drugs, and Biological agents.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Rheumatoid Arthritis (RA) causes, stages, symptoms, diagnosis, and specific joint affection
Chronic Low Back Pain diagnosis, symptoms, treatment and Seronegative Spondyloarthritis types