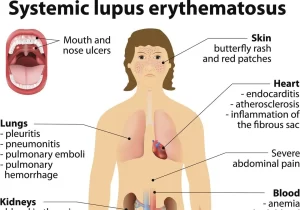
Systemic Lupus Erythematosus symptoms, diagnosis, types and treatment
Systemic Lupus Erythematosus is a chronic relapsing inflammatory multisystemic disorder of connective tissue characterized by involvement of the skin, joints, and serosal membranes. It is of unknown etiology but is thought to represent a failure of the regulatory mechanisms of the autoimmune system (Breakdown of self-tolerance).
Epidemiology
- Prevalence worldwide: 2-140/100,000 worldwide but as high as 207/100,000.
- Incidence: 1-10/100,000 worldwide.
- Population at high risk: Women in their reproductive years. Female: Male ratio is approximately 9: 1 (Female > Male) post-puberty and menopausal.
- Variation in race and ethnicity: More common in Black (3-6 X), Hispanic and Native Americans (2-3 X) and Asian (2X) populations.
- Cost: There are direct costs associated with treatment (Eg: 100 Billion $ in healthcare costs associated with auto-immune diseases) and indirect costs related to lost productivity and wages.
Aetiology
The cause is unknown, but there are several predisposing factors. Studies on patients suggest that SLE is caused by genetically determined immune abnormalities that can be triggered by both exogenous and endogenous factors.
Genetic background
- There is a higher concordance rate in monozygotic twins (up to 25%) compared to dizygotic twins (3%).
- Familial aggregation: First-degree relative 12%.
- There is a stronger association with HLA DR2 and DR3.
- There is an inherited deficiency of complement (C2, C4 & C1q).
Environmental factors (environmental triggers)
Ultraviolet light (B component): Flare of SLE in 70% of patients (Due to increased cellular remnants in SC tissues after sun exposure).
Possible:
1. Gender and Hormones:
Estrogen H increases the risk. Androgens decrease the risk. Females are at higher risk due to:
- Increased antibody response more than males.
- Oral contraceptive pills (OCPs) and Hormone replacement therapy (HRT): Increases the risk (1.2-2 Folds).
- Estradiol binds to T and B Cells: Increases activation and survival causing prolonged immune response.
2. Infections:
- Induce B and T Cells that recognize Auto antigens forming Auto antibodies.
- EBV: More common in SLE patients. Activate B cells. Produces amino acid sequences that mimic some of DNA.
3. Drugs: Hydralazine, Procainamide, methyldopa.
Notes
- Triggering factors may increase oxidative stress with subsequent apoptosis with expression of previously hidden antigens on the cell surface where they become immunogenic.
- SLE is characterized by widespread immune complex deposition inflammation and vasculitis.
- Fibrinoid (eosinophilic material) is found along blood vessels and tissue fibers.
Phases of disease pathogenesis
Initiation:
- Multiple proposed mechanisms that may vary from patient to patient.
- Occurs years prior to the onset of clinical symptoms.
Amplification and perpetuation of dysregulated immune mechanisms response of target organs to inflammatory insults.
Irreversible damage: from disease and secondary effects of treatment.
Organ damage
Organ Occurs due to Immune complex Deposition, Formation, and Interaction. Cytokines involved in tissue injury/organ damage in lupus include:
- B cell maturation and survival cytokines: B lymphocyte stimulators (Blys/BAFF).
- Increases Interleukin-6,17,18.
- Increased Pro-inflammatory mediators: Type 1 and 2 Interferons (IFNs).
Raynaud’s phenomenon
A characteristic sequence of digital pallor due to vasospasm followed by cyanosis due to the presence of deoxygenated blood, then rubber due to reactive hyperaemia. Capillary fallout on capillary ophthalmoscopy distinguishes secondary Raynaud’s from primary Raynaud’s.
Mucocutaneous features
Skin provides one of the best windows through which we view the activity of lupus and we establish the diagnosis.
Mucous Membranes (Oral OR Nasal ulcers):
- Oral: Palate, Buccal, and Tongue.
- Nasal ulcers
- In the absence of Vasculitis, Behcet’s disease, Infection (Herpesvirus), Inflammatory bowel disease (IBD), Reactive arthritis and Acidic food.
Cutaneous
Acute cutaneous lupus:
- Lupus Malar rash.
- Bullous lupus.
- TEN variant of SLE
- Maculo- papular lupus rash.
- Photo-sensitive lupus rash (In the absence of Dermato-myositis).
Sub-acute cutaneous lupus:
Non-indurated Psoriaform and/or Annular polycyclic lesions that resolve without scarring.
Chronic cutaneous lupus:
- Classic discoid rash: Localized (Above the neck) or Generalized (Above and Below the neck).
- Hypertrophic (Verrucous) lupus.
- Lupus profundus (Panniculitis).
- Lupus affects the fat underlying skin.
- Mucosal lupus.
- Chilblain lupus.
- Discoid lupus/ Lichen planus overlap.
- Lupus Erythematosus Tumidus.
- Vasculitis.
Symptoms
- Lupus Malar rash: Fixed erythema, flat or raised over the malar eminences tending to spare the nasolabial folds.
- Bullous lupus: Bullous systemic lupus erythematosus (BSLE) is a rare autoimmune blistering disorder that typically manifests as an acute vesiculobullous eruption in a patient with known systemic lupus erythematosus (SLE).
- TEN variant of SLE: Toxic epidermal necrolysis (TEN)-like lesions are an infrequent clinical presentation of SLE that presents with photo-distributed exanthema and minimal mucositis and the onset of the rush is insidious.
- Maculo-papular lupus rash.
- Photosensitivity rash: Abnormal reaction to sunlight.
- Non-Indurated Psoriaform and/or Annular polycyclic lesions that resolve without scarring.
- Classic discoid rash: Localized (Above the neck), and Generalized (Above and Below the neck).
- Hypertrophic (Verrucous) lupus: It is a rare type of chronic cutaneous lupus erythematosus characterized by the appearance of lesions on sun-exposed areas (frequently the extensor surfaces of forearms, face, and upper trunk) which vary from squamous violet, painful papules and blackish hyperkeratotic ulcers to depigmented atrophic plaques on the back, hyperkeratotic papules on upper extremities, and disseminated keratoacanthoma-like papulonodular verrucous lesions.
- Lupus Profundus (Panniculitis): Lupus affecting the fat underlying skin aka lupus panniculitis
- Mucosal lupus.
- Discoid lupus/Lichen planus overlap.
- Chilblain lupus: Painful inflammation of small blood vessels. It is characterized by red or violaceous papules and plaques located on acral areas, Cold temperatures, particularly moist cold climates, precipitate the lesion.
- Lupus Erythematosus Tumidus: Tumidus is the Dermal form of lupus. Characteristically photo-sensitive, Red, Swollen, Urticaria like: Bumps and Patches. and Ring-shaped (Annular).
- Vasculitis: Levido reticularis: Also seen in antiphospholipid syndrome, Nail fold infarct. Palpable purpura, Digital ulceration, Splinter hemorrhage.
- Alopecia: it associates with active disease. It’s either: Diffuse alopecia which is reversible after disease activity is controlled (Non-scarring alopecia: Diffuse thinning or Hair fragility with visible Broken hair), OR Discoid disease causes patchy hair loss which is permanent.
Lupus on the outside
- Synovitis.
- Discoid rash.
- Malar rash.
- Oral ulcer.
- Subacute cutaneous lupus erythematosus.
- Vasculitis.
- Lupus profundus.
Lupus on the inside
- Serositis.
- Brain atrophy.
- Pericardial effusion.
- Cerebral infarct.
- Spherocytes.
- Glomerulonephritis.
Life-threatening complications
- Cutaneous digital Gangrene.
- Cutaneous Necrosis.
- Thrombocytopenia.
- Autoimmune haemolytic anemia.
- Catastrophic antiphospholipid syndrome.
- Pericardial tamponade.
- Myocarditis.
- Pulmonary alveolar haemorrhage.
- Myelitis.
- Mesenteric vasculitis.
Diagnosis:
CBC
- Anaemia: Autoimmune hemolytic anaemia: indices of hemolysis, Coomb’s test is positive, Anemia of chronic disease, Blood loss, Drugs, and Renal insufficiency.
- Antibody-mediated leucopenia, lymphopenia, thrombocytopenia.
ESR
- Elevated in active lupus.
- It does not reflect disease activity.
- It may remain elevated in remission.
CRP
- Not a reliable indicator.
- It is often normal unless there is serositis or infection.
Autoantibodies
Anti-Nuclear Antibody (ANA):
- Has high sensitivity and low specificity.
- The best screening test.
- Repeated negative tests make SLE unlikely.
- Can be positive in up to 10-15% of normal individuals.
- Immuno-fluorescent technique (lF) is more reliable than ELISA and/or bead assays (IF> ELIZA).
Anti-double-stranded DNA (Anti-ds DNA):
- High titers are specific.
- Has a 60% sensitivity.
- In some patients, it correlates with disease activity (Nephritis and Vasculitis).
Anti-Smith (Anti-Sm):
- Specific to SLE.
- More common in Blacks and Asians.
- No definite clinical correlation.
Anti-phospholipid antibodies: Women with childbearing potential and SLE should be screened for both Anti-phospholipid and anti-Ro antibodies.”
Anti Ro/SS-A:
- Non-specific.
- Associated with Sicea syndrome, Neonatal lupus, and Sub-acute cutaneous lupus.
- Associated with decreased risk for Nephritis.
Anti RNP:
- It is non-specific.
- Associated with RA (Rhupus).
- It is more common in black than in White (Black > White).
Anti La/SS-B:
- Decreased risk for Nephritis.
- It is associated with anti-Ro.
Anti-Histone: Common in Drug-induced lupus.
Anti-erythrocyte: It is measured by DCT (Direct Coombs Test).
Anti-platelet: It is not useful clinically.
Anti-neuronal: It is positive in CSF affection: Active CNS Lupus.
Anti-ribosomal P: Positive in serum due to: Depression and Psychosis in lupus.
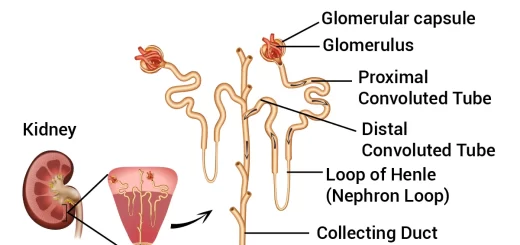
Investigations for specific organ involvement
a. Monitoring lupus nephritis:
- 24h urine protein.
- Serum complement level.
- Anti-dsDNAxiter.
- Renal function: blood urea, S. creatinine, creatinine clearance.
b. CNS:
- CSF-EEG: non-specific.
- CT scan–MRI: diagnose vasculitis-thrombosis.
- Autoantibodies: antiphospholipid: focal manifestations. Antineuronal: diffuse manifestations
- Antiribosomal P: psychiatric lupus.
c. Pulmonary: chest x-ray-CT scan.
d. Cardiac: chest x-ray-echocardiography.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
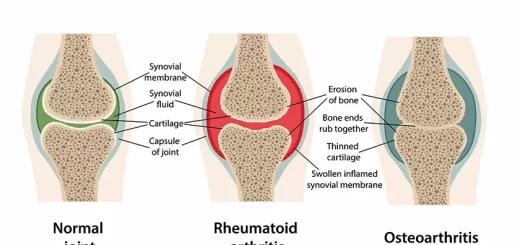
Rheumatoid Arthritis (RA) causes, stages, symptoms, diagnosis, and specific joint affection
Rheumatoid Arthritis diagnosis and treatment, Disease-Modifying antirheumatic drugs (DMARDs)
Non-radiographic axial spondyloarthritis, Reactive arthritis, and Enteropathic arthritis