Benign prostatic hyperplasia (BPH), TRUS biopsy, Prostate disease symptoms and treatment
Diseases of the prostate
- Inflammations.
- benign prostatic hyperplasia.
- malignant tumors.
Benign prostatic hyperplasia (BPH)
- COMMON
- Old age
- Androgen-dependent growth of stromal and glandular elements.
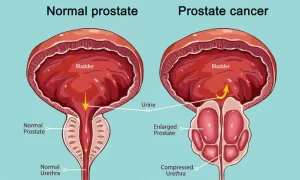
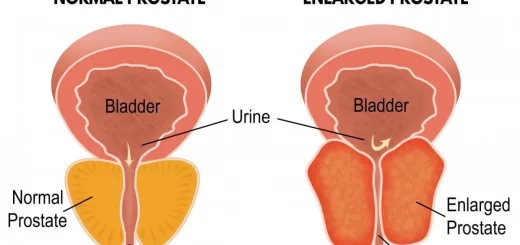
- Inner transitional zone of the bladder leading to Compression of the urethra
- C/P. urinary obstruction, frequency, incomplete emptying.
- Complications: obstructive uropathy- azotemia- infections-bladder hypertrophy and
- bladder diverticulae.
- NOT premalignant.
Pathogenesis
Dihydrotestosterone (DHT), the ultimate mediator of prostatic growth, is synthesized in the prostate from circulating testosterone by the action of the enzyme 5a-reductase type 2 (in the stromal cells). DHT binds to and activates androgen (ARS) found in both stromal and epithelial prostate cells. It is more potent than testosterone because it has a higher affinity for ARS and forms a more stable complex with them.
Binding of DHT stimulates ARS to translocate from the cytoplasm to the nucleus and activate the transcription of androgen-dependent genes, which encode several growth factors and their receptors. (FGF) (TGF-β), Although the ultimate cause of BPH is unknown, it is believed that DHT-induced growth factors act by increasing the proliferation of stromal cells and decreasing the death of epithelial cells.
Morphology
- Gross appearance of BPH: The prostate is enlarged, weighing (60- 100gm), The Cut surface of the gland shows well-defined nodules with small cystic spaces (arrow). These nodules are concentrated in the periurethral area (transition zone). causing slit-like narrowing of the urethra.
- The whole mount views a prostatectomy specimen with BPH: showing nodules of hyperplastic glands on both sides of the urethra.
The nodular appearance can be appreciated (arrow in A), There is hyperplasia of both the glands and the fibromuscular stoma, On the high power view, there are aggregates of small to cystically dilated glands lined by 2 layers of cells an inner columnar and an outer cuboidal or flattened epithelium, The glandular lumina often contain laminated proteinaceous secretory material (Corpora amylacea).
Clinical picture and complications
- Urinary frequency, nocturia, difficulty in starting and stopping the stream of urine, overflow dribbling, and dysuria.
- The increased resistance to urinary outflow leads to bladder hypertrophy and distention, accompanied by urine retention.
- The inability to empty the bladder completely creates a reservoir of residual urine that is a common source of infection leading to an increased risk of developing bacterial infections of the bladder and kidney.
- Repeated infections…….Hydroureter/ hydronephrosis.
- In many cases, sudden, acute urinary retention occurs that requires emergency catheterization for relief.
Treatment
- Medical: α-adrenergic blockers (Flomax) (decrease prostate smooth muscle tone), Sα reductase inhibitors (Finasteride)( Shrink the prostate by decreasing DHT).
- Surgical: TURP.
Prostatic adenocarcinoma
- Most common cancer in men (over 50).
- However, it causes less than 10% of cancer deaths.
- Wide range of clinical behavior.
- Etiology, Age, race, environmental, family, history, androgens. GENES.
- The most common driver mutations are gene rearrangements causing androgen-dependent overexpression mostly belonging to the ETS family (most commonly ERG or ETV1).
- Peripheral in location (NO urinary symptoms), Mass can be felt by DRE. Precursor lesion: PIN (prostatic Intra-epithelial neoplasia).
Diagnosis
TRUS biopsy
Small crowded glands tightly packed and lined by a single layer of cells. Cells have large nuclei and prominent nucleoli.
Spread
- Local invasion to periprostatic tissue, seminal vesicles, and the base of the urinary bladder, which may produce ureteral obstruction.
- Lymphatic spread to the obturator nodes and eventually to the para-aortic nodes.
- Hematogenous spread occurs chiefly in the bones, particularly the axial skeleton. Bony metastases are typically osteoblastic.
- The bones most commonly involved are lumbar spine, proximal femur, pelvis, thoracic spine, and ribs.
- Tumors may also spread to the viscera, but extensive visceral dissemination is the exception rather than the rule.
Prognosis
- Grade and stage are the most important prognostic factors in prostate cancer.
- Grading is performed using the Gleason System.
- Most potentially treatable cancers detected on needle biopsy as a result of screening have Gleason scores of 6 or 7.
- Tumors with Gleason scores of 8 through 10 tend to be advanced cancers that are less likely to be cured.
- T1 tumors are tumors that are not detected clinically by DRE or by imaging.
Treatment
- Watchful waiting: A number of genomic tests using gene panels have recently been developed that may enhance the ability to predict which cancers (e.g. low-volume Grade Group 1) can be followed by active surveillance alone.
- Surgery: Radical Prostatectomy.
- Radiation therapy
- Hormonal therapy (androgen deprivation): achieved by bilateral orchiectomy or by or by administration of synthetic analogs of luteinizing hormone-releasing hormone (LHRH).
PSA
- Product of prostatic epithelium…normal constituent in semen. In normal men, only minute amounts of PSA circulate in the serum.
- PSA is organ-specific, but not cancer-specific.
- Elevated blood levels of PSA occur in association with localized as well as advanced cancer.
- PSA can also be increased in BPH, prostatitis, and prostate gland infarction (e.g., in the setting of BPH), instrumentation of the prostate, NOT advised to be used for screening (many prostate cancers are indolent).
- Evaluation of PSA concentrations after treatment has great value in monitoring progressive or recurrent disease.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Enlarged prostate symptoms, Prostatic artery embolization (PAE) importance & risks
Prostate function, structure, lobes, Benign enlargement of prostate & malignant prostatic tumor
Nephroblastoma (Wilm’s tumor), Risk factors of Urothelial tumors (Tumors of transitional epithelium)
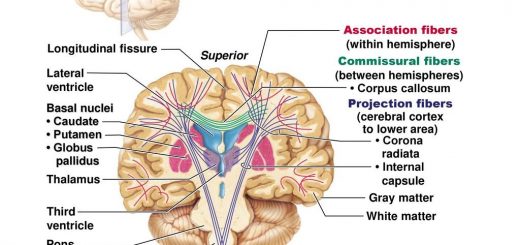
Urinary bladder structure, function, Control of micturition by Brain & Voluntary micturition
Urinary system structure, function, anatomy, organs, Blood supply & Importance of renal fascia
Histological structure of kidneys, Uriniferous tubules & Types of nephrons