Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
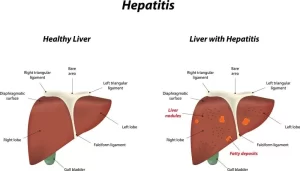
Hepatitis refers to the inflammation of the liver processes nutrients, filters the blood, and fights infections, When the liver is inflamed or damaged, its function can be affected, Many people with hepatitis do not have symptoms and do not know they are infected, when symptoms occur with an acute infection, they can appear anytime from 2 weeks to 6 months after exposure.
Acute Hepatitis
Symptoms of acute hepatitis include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, light-colored stools, joint pain, and jaundice, Symptoms of chronic viral hepatitis can take decades to develop.
Causes
- Viral: Hepatotrophic: A, B, C, D, E. Non-Hepatotrophic: CMV, EBV.
- Ischemic.
- Drug-induced.
- Autoimmune.
Causes of viral hepatitis
Common
- Hepatitis A
- Hepatitis B ± hepatitis D
- Hepatitis C
- Hepatitis E
Less common
- Cytomegalovirus
- Epstein-Barr virus
Rare
- Herpes simplex
- Yellow fever
Clinical picture
- Asymptomatic: Only elevated transaminases.
- Anicteric: GI and influenza-like symptoms, No jaundice.
- Classic: 3 stages:
- Prodromal 3-4 days: Profound malaise, fever, anorexia nausea, vomiting, abdominal pain. The most important pronouncing features are malaise, anorexia, and vomiting.
- Icteric 1-4 weeks: Change of urine color followed by jaundice and itching, Change in urine color precedes jaundice and itching by 1-2 days, The patient feels generally better, and his appetite returns, Tender hepatomegaly.
- Convalescent
Complications of acute hepatitis
Prolonged cholestasis: Classic acute hepatitis but the icteric stage is prolonged 8-29, weeks with manifestations of cholestasis, More with HAV.
Fulminant hepatitis: The patient after a typical acute onset becomes deeply jaundiced, ominous manifestations, persistent vomiting, fetor hepaticus, drowsiness, flappy tremors, and finally coma, Rare in HCV but more common in HAV, Usually in acute hepatitis when jaundice appears, vomiting stops but in fulminant hepatitis when jaundice appears, vomiting doesn’t stop.
Relapse: 1.8-15% especially HAV. The attack is usually milder. Precipitated by premature activity.
Post-hepatitis syndrome: Usually, this is a matter of weeks but it may extend to months, Features are anxiety, fatigue, failure to regain weight, anorexia, and right upper abdominal discomfort, The liver edge may be palpable and tender, All investigations are ok but the patient still complaining of a complaint of acute hepatitis which is a post-hepatitis syndrome, Treatment consists of reassurance after a full investigation.
Diagnosis
1. SGOT, SGPT: peak levels 1-2 days before or after onset of jaundice.
- Levels > x 10 ULN.
- If this level is less than 10 times has 2 possibilities: Resolving acute hepatitis which is anicteric and asymptomatic, and Form of chronic hepatitis, Useful in early diagnosis and detection of anicteric cases.
2. Bilirubin & ALP are usually elevated.
3 PT prolonged
Treatment
1. Bed rest: (The most important) to give rest to the inflammatory organ (the liver).
2. Diet: low-fat high carbohydrate diet more palatable to the patient.
3. Symptomatic and supportive treatment: Treat the fever and vomiting with antipyretic and antiemetic, respectively. Convalescence is not allowed till the patient is symptom-free & bilirubin <1.5 mg/dl.
HAV
- RNA virus.
- Oral-fecal transmission.
- Incubation period: 15 to 45 days.
- Jaundice > 70% in adults.
- Fulminant hepatic failure < 1%.
- Peak infectivity occurs 2 weeks before and at least 1 week after the initial symptoms.
- No chronicity.
- Vaccination is available.
- The diagnostic tests for diagnosis of acute hepatitis A are (IgG, IgM, and anti-HAVAb).
- If IgM is negative and IgG is positive and the patient is with hepatitis, this is past hepatitis A infection and the acute hepatitis is due to other causes).
Chronic hepatitis
Definition
- Persistent inflammatory reaction in the liver for more than 6 months.
- Clinically: Suspected from persistently elevated hepatic transaminases (necro-inflammatory markers) for > 6 months.
- Histologically: Liver biopsy is the gold standard for diagnosis.
Etiology
- Viral: B & D, C, and sometimes hepatitis E but very rare.
- Autoimmune.
- Drugs.
- Genetic: Wilson’s disease, hemochromatosis, alpha 1 anti-trypsin deficiency.
- Alcohol (ASH).
- Fatty infiltration (NASH).
Liver biopsy
The gold standard for diagnosis of hepatitis and evaluation of severity of liver disease.
Evaluation includes:
- Grading: necro-inflammatory changes.
- Staging: the extent of fibrosis.
- The most commonly used currently is the METAVIR system, which grades inflammation from 0 to 4 (A 0-4) and stages fibrosis from 0 to 4 (F0-4).
Specific findings for specific etiology e.g:
- Mallory hyaline bodies in alcoholic hepatitis.
- Plasma cell infiltration in AIH.
- Ground glass hepatocyte in HBV.
- PCR for the virus in liver tissue.
- The hepatic concentration of Cu and Fe in Wilson and hemochromatosis.
Clinical picture
- Symptoms: Asymptomatic. Only presented with elevated transaminase.
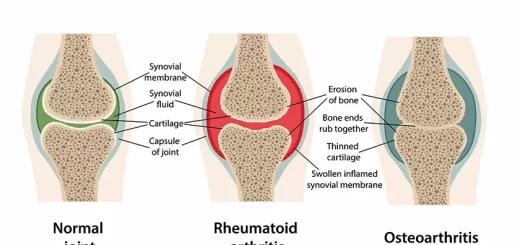
- Fatigue (most common), rt hypochondrial pain, nausea, jaundice, muscle, and joint pains.
- You should start diagnosis of the cause of chronic hepatitis if these enzymes are elevated for more than 6 months.
Signs
Tender hepatomegaly, occasionally vascular spiders.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Histological structure of gallbladder & Pancreas, Functions of the liver & Composition of bile
Portal Venous System, Histological structure of Liver, portal vein and its tributaries
Histology of pancreas, Structure of islets of Langerhans, Insulin function & Metabolism
Liver development, congenital anomalies, function & Pancreas development