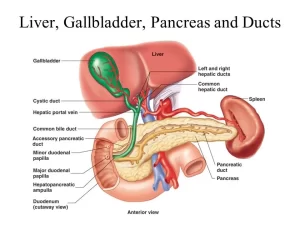
Histological structure of gallbladder and Pancreas, Functions of the liver and Composition of bile
The gallbladder is part of your digestive system, It is a small, pear-shaped organ located under your liver that stores and releases bile, the liver produces bile that helps digest fats in the food you eat. It is located in the upper right part of your abdomen (belly), Bile helps your digestive system break down fats, it is a mixture of cholesterol, bilirubin, and bile salts.
Histological structure of gallbladder
It is a hollow, pear-shaped organ attached to the lower surface of the liver, The histological organization of the gallbladder is adapted to its function of storage/concentration of bile and its release when needed into the duodenum, The wall of the gallbladder consists of:
Mucosa
Highly folded particularly when the gallbladder is empty. It is lined by simple columnar epithelium with apical microvilli adapted for salt and water absorption. The lamina propria is vascular and rich in lymphocytes and plasma cells.
Musculosa
It is relatively a thin layer. It is formed of bundles of smooth muscle fibers oriented in several directions and separated by fibro-elastic connective tissue.
Adventitia or Serosa: according to anatomical surface.
Histological structure of the exocrine pancreas
The pancreas is classified as a mixed gland; composed of both endocrine (pancreatic islets of Langerhans) and exocrine parenchyma.
Histological organization of the pancreas
I- The stroma
Thin connective tissue capsule and thin septa that divide the pancreas into small lobules and carry with them the vascular and nervous supply. Network of reticular fibers that support the pancreatic parenchyma.
Il- The endocrine parenchyma of the pancreas.
IIl- The exocrine parenchyma of the pancreas
It is a compound tubuloalveolar (tubuloacinar) gland secreting digestive enzymes.
A. The pancreatic acini:
- They are serous acini, oval in shape and larger than those of the salivary glands without myoepithelial cells.
- The acini are tightly-packed, pressing against one another thus acquiring variable shapes.
- Each pancreatic acinus is lined by tall pyramidal cells and has a characteristic staining pattern, with its prominent peripheral deep basophilia (due to abundant rER) and central eosinophilia (due to zymogen granules).
- The lumen of each pancreatic acinus is characteristically narrow and lined by flat centroacinar cells. They represent the first part of the intralobular ducts (intercalated ducts), that is telescoped inside the lumen of the acinus.
B. The pancreatic duct system
- The intralobular ducts: its proximal part is forming the centroacinar cells. The remaining short intercalated part is lined by low cuboidal cells.
- The interlobular ducts: are present in the connective septa between the lobules and are lined by simple cuboidal then simple columnar cells.
- The main pancreatic duct: large duct with a wider lumen. It is lined by simple columnar cells with goblet cells, a lining that is similar to that of the duodenum where it opens.
Physiology of the Liver
The liver is the largest gland of the body.
Functions of the liver
I. Digestive function: formation and secretion of bile
II. Non-digestive functions:
- It acts as a blood reservoir and as a mean of transferring blood from the portal to systemic circulation, A normal volume of about 350 ml of blood is found in the organ, An additional liter may be stored in the organ and transferred to the systemic circulation.
- The liver serves as a filter between the blood coming from the gastrointestinal tract and the blood in the rest of the body through the activity of phagocytic reticuloendothelial cells (Kupffer cells), found in the sinusoids.
- The production of red blood cells is a normal function of the fetal liver.
- Destruction of aged red blood cells by the activity of kupffer cells.
- Excretion of bile pigments.
- Detoxification function: The liver inactivates toxins, hormones, and steroids that might be harmful to the body by oxidation, hydroxylation, and other reactions mediated by the large number of cytochrome P450 enzymes expressed in hepatocytes. Ultimately, metabolites are secreted into the bile for elimination via the gastrointestinal tract.
- Metabolic functions: The liver plays key roles in carbohydrate, fat, and protein metabolism, For example, it plays a major role in maintaining the stability of blood glucose levels in the postprandial period, removing excess glucose from the blood and returning it as needed – the so-called glucose buffer function of the liver, In addition, the liver preserves cholesterol homeostasis by synthesizing this molecule and also converting excess cholesterol to bile acids.
- Storage of iron and vitamins.
- Endocrine function: synthesis of erythropoietin, somatomedins, etc.
- Helps in blood clotting mechanism (synthesis of clotting factors)
- Synthesis of plasma proteins such as acute phase proteins, albumin, hormone binding proteins, etc.
The functional unit of the liver is the hepatic lobule.
Bile secretion
Bile is secreted by the cells of the liver into the bile duct, which pours its secretion into the duodenum. Bile is considered as a secretion because it contains bile salts which serve many important functions in the body, and excretion because it contains waste products such as bile pigments.
In between the meals, the sphincter of Oddi is closed, bile flows, and is stored in the gall bladder whose wall has a concentrating power that enables it to store a large volume. After food intake, the sphincter of Oddi relaxes, the gall bladder contracts, and both diluted bile coming from the liver and concentrated bile coming from the gall bladder are evacuated into the duodenum.
Composition of bile
The volume of bile is about 500 ml/day, The bile pigments, bilirubin, and biliverdin, are responsible for the golden yellow color of bile. In the gall bladder bile is acidified by the reabsorption of its NaHCO3 content, The acidic medium prevents the precipitation of calcium and gall stone formation.
The specific gravity of gall bladder bile is 1050 while that of liver bile is 1008. Some of the constituents of bile are reabsorbed in the intestine and secreted again by the liver (enterohepatic circulation).
The main constituents of bile are:
- Water.
- Bile salts.
- Bile pigments.
- Cholesterol.
- Fatty acids.
- Lecithin.
- Phosphatidylcholine.
- Alkaline phosphatase.
- Electrolytes: Cations as Na+, K+, Ca++, Anions as Cl−, HCO3−.
- Mucin-like substances.
Differences between human hepatic duct bile and gall bladder bile
Hepatic Duct Bile:
- Percentage of solids: 2-4
- Bile acids (mmol/L): 10-20
- pH: 7.8 – 8.6
- Specific gravity: 1008
Gall bladder Bile:
- Percentage of solids: 10-12
- Bile acids (mmol/L): 50-200
- pH: 7.0-7.4
- Specific gravity: 1050
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Portal Venous System, Histological structure of Liver, portal vein and its tributaries
Histology of pancreas, Structure of islets of Langerhans, Insulin function & Metabolism
Small intestine function, anatomy, parts, Arterial supply of the duodenum, midgut & hindgut
Pancreas function, anatomy, parts, relations, ducts & blood supply
Stomach parts, function, curvatures, orifices, peritoneal connections & Venous drainage of Stomach