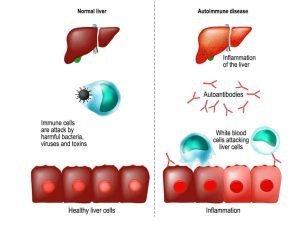
Autoimmune Hepatitis symptoms, types, diagnosis, causes and treatment
AIH (autoimmune hepatitis) is an irreversible chronic liver disease, During its course, remissions and relapses may occur, Remission (no symptoms and normal lab investigations) may occur spontaneously or induced by a drug, Relapses occur at certain periods which cannot be expected so long life drugs must be taken.
Autoimmune Hepatitis
Prevalence of AIH ranges from 15 to 25 cases per 100,000 inhabitants in Europe and is increasing in both sex (3:1) (more in female), Any age with a bimodal distribution usually peaks around puberty and between the 4th and 6th decade although a significant proportion of patients are even older (above 65 years of age).
Clinical picture
Broad range from asymptomatic (just abnormal liver function test) to (acute/severe)or even fulminant, Most common clinical phenotype of the disease is characterized by an insidious onset:
- Fatigue, general ill health.
- Right upper quadrant pain.
- Lethargy, malaise.
- Anorexia, weight loss, nausea
- Pruritus, fluctuating jaundice.
- Polyarthralgia involving the small joints.
- May be associated with other autoimmune diseases.
Types
There are three types according to Abs in the circulation:
AIH-1
- The more frequent type of AIH (90%).
- Detection of ANA (antinuclear Abs), SMA (smooth muscle Abs), or (anti-SLA/LP (soluble liver Ag).
- Association with HLA DR3, DR4, and DR13.
- Any age at onset.
- Variable clinical and histopathological severity.
- A rare failure of treatment but variable relapse rates after drug withdrawal
- Variable need for long-term maintenance therapy.
AIH-2
- 10% of AlH cases (rare).
- Detection of anti-LKM1 (liver kidney microsomal), anti-LC1, and rarely anti-LKM3.
- Association with HLA DR3 and DR7.
- Onset usually in childhood and young adulthood.
- Clinical and histopathological severity is commonly acute and advanced.
- Frequent failure of treatment and frequent relapse rates after drug withdrawal.
- The need for long-term maintenance therapy is very common.
AIH-3
- SLA/LP positive.
- Otherwise very similar to AIH-1 Possibly more severe.
- Ro52-antibody is positive.
Diagnosis
Simplified diagnostic criteria of the International Autoimmune Hepatitis Group (Definite AIH: ≥ 27, Probable AIH: ≥ 6)
Elevated IgG
- IgG above the normal limit. → 1 point.
- IgG 110 times above the normal limit. → 2 points.
Autoantibodies
- ANA or ASMA ≥ 1.40 → 1 point.
- ANA or ASMA ≥ 1.80 → 1 point
- LKM ≥ 1.40 → 2 points
- SLA/LP positive → 2 points
Histology of Chronic Hepatitis
- Compatible with AIH. → 1 point.
- Typical of AlH. → 2 points
Absence of viral hepatitis → 2 points
Points ≥ 6 PROBABLE AIH, Points ≥ DEFINITE AIH
Definite AIH
- Normal alpha-1AT phenotype (exclude alpha 1AT deficiency).
- Normal ceruloplasmin level (exclude Wilson disease).
- Normal iron and ferritin levels (exclude hemochromatosis).
- No active hepatitis A, B, or C infection.
- Daily alcohol < 25 g/d.
- No recent hepatotoxic drugs.
- Predominant AST/ALT abnormality (not cholestatic pattern).
- Y-globulin or IgG level >1.5 times the upper limit of normal.
- Titer ANA, SMA, anti-LKM1 > 1:80 in adults and >1:20 in children.
- AMA (anti-mitochondrial Ab) negative (which is specific to PBC).
liver histology
- Interface hepatitis is moderate to severe.
- No biliary lesions, granulomas, or prominent changes suggestive of another disease.
Probable AIH
- Partial alpha-1AT deficiency.
- Non-diagnostic ceruloplasmin level.
- Non-diagnostic iron and/or ferritin changes.
- No active hepatitis A, B, or C infection (B,C may be present).
- Daily alcohol <50 g/d.
- Recent hepatotoxic drugs.
- Predominant AST/ALT abnormality.
- hypergammaglobulinemia of any degree.
- ANA, SMA, anti-LKM1>1:40 in adult.
- Other autoantibodies.
liver histology
- Interface hepatitis is moderate to severe.
- No biliary lesions, granulomas, or prominent changes suggestive of another disease.
Treatment proposal for adult patients with AIH (e.g., 60 kg)
- Treatment should be continued for at least 3 years and for at least 24 months after complete normalization of serum transaminases.
- (ALT levels <ULN, IgG levels < 12 g/L were highly predictive for successful treatment withdrawal) (biochemical remission).
- Performance of a liver biopsy prior to treatment withdrawal is advisable as histological findings are predictive of fibrosis progression and relapse.
- Alternative drug therapies for unsatisfactory responses:
- Second-line immunosuppressive therapy includes MMF (mycophenolate mofetil) and CNI (Calcineurin inhibitors).
- Their major benefits are potent immunosuppressive activity with a rapid onset of action but these agents exhibit their own side effects.
- If the patient comes in late stage has liver failure.
- Liver transplantation is the best choice in this case which is curable with only 4-5% of relapse.
You can subscribe to science online on Youtube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Primary biliary cirrhosis symptoms, cause, diagnosis, treatment, and Osteoporosis
Diagnosis of the cause of jaundice, Hepatobiliary imaging, treatment of cholestasis and Pruritus
Liver Cholestasis types, causes, features, symptoms, diagnosis, and treatment
Conjugated hyperbilirubinemia cause, symptoms and treatment
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer