Liver Cirrhosis causes, symptoms, treatment and stages, Liver Biopsy and treatment of PHTN
The liver consists of 2 main lobes: right and left. Both are made up of 8 segments, The smallest unit of the liver is the hepatic lobule which is bounded by fibrous tissue septae and a special layer of liver cells called a limiting end plate, both support and preserve the intact of liver lobule.
Liver cirrhosis
There is a difference between acute and chronic liver injury.
- Acute liver injury: the lobule boundaries remain intact so the regeneration of liver cells will be faster and get back to normal as if nothing happened.
- Chronic liver injury: there will be destruction of the boundaries of hepatic lobules so the regeneration will be haphazard and will form regenerative nodules and loss of normal hepatic architecture.
Chronic liver injury → collagen → fibrosis → destruction of the boundaries → deposition of abnormal nodules.
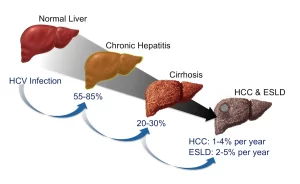
Cirrhosis is a diffuse hepatic process characterized by fibrosis and the conversion of normal liver architecture into abnormal nodules, Cirrhosis represents the final common histologic pathway for a wide variety of chronic liver diseases, The progression of liver injury to cirrhosis may occur over weeks to years, Indeed, patients with hepatitis C may have chronic hepatitis for as long as 40 years before progressing to cirrhosis.
Morphological classification
1. Micronodular cirrhosis:
- Characterized by thick, regular septa, by regenerating small nodules varying little in size, and by the involvement of every nodule.
- Nodular variation < 3mm.
- Example: Alcoholic cirrhosis.
2. Macronodular cirrhosis:
- Characterized by septa and nodules of variable sizes and by normal lobules in larger nodules.
- Nodular variation> 3mm.
- Example: Hepatitis B & C.
3. Mixed cirrhosis.
Metavir scoring system (stages preceding liver cirrhosis):
- F1: deposition of collagen around the portal tract.
- F2: portal fibrosis with few septa toward the central vein.
- F3: numerous septa with bridging around the central vein.
- F4: cirrhosis and formation of regenerative nodules.
Etiology of liver cirrhosis
- Viral hepatitis (B, C, D).
- Autoimmune chronic hepatitis.
- Alcohol.
- Drug-induced (methotrexate, amiodarone).
- Cryptogenic. (can’t reach the cause).
- Metabolic (Non-alcoholic steatohepatitis (fatty liver), hemochromatosis (deposition of iron), Wilson’s disease (deposition of copper), alpha 1- antitrypsin deficiency, type IV glycogenosis).
- Cholestatic (Primary biliary cirrhosis, Primary sclerosing cholangitis).
- Hepatic venous outflow obstruction (veno-occlusive disease or sinusoidal obstructive syndrome (at the level of hepatic sinusoids), Budd-Chiari syndrome.
Pathophysiology of fibrosis
The development of fibrosis reflects an alteration in the balanced processes of extracellular matrix production and degradation. The extracellular matrix, the normal scaffolding for hepatocytes, is composed of collagens especially type I, III, and V, glycoproteins, and proteoglycans.
Stellate cells, normally located in the perisinusoidal space, are essential to produce extracellular matrix, Stellate cells, which were once known as Ito cells, lipocytes or perisinusoidal cells may become activated into collagen-forming cells by a variety of paracrine factors.
Such factors may be released by hepatocytes, Kupffer cells, and sinusoidal endothelium following liver injury, As an example, increased levels of the cytokine transforming growth factor beta 1 (TGF-beta 1) are observed in patients with chronic hepatitis C and those with cirrhosis, TGF-beta 1, in turn, stimulates activated stellate cells to produce type I collagen.
Increased collagen deposition in the space of Disse (the space between hepatocytes and sinusoids) and the diminution of the size of endothelial fenestrae lead to the capillarization of sinusoids, Activated stellate cells also have contractile properties, Both capillarization and constriction of sinusoids by stellate cells contribute to the development of PHTN.
The normal function of stellate cells (Ito cell, lipocytes) is/fat storage, Once it is injured, its character and morphology change into active stellate cells, The changes are: Increase proliferation, Contractility function, Having a role in fibrogenesis, and WBC chemoattraction.
Clinical features
Cirrhosis results in two major clinical events:
- Manifestations of hepato-cellular failure.
- Manifestations of portal hypertension.
- In some diseases, the manifestations of PHTN are more prominent than hepato-cellular failure as in schistosomal hepatic fibrosis which is manifested by splenomegaly and esophageal varices.
- On the other hand, the manifestations of hepato-cellular failure are more prominent in viral hepatitis C.
Clinically, Cirrhosis is classified into compensated and decompensated liver cirrhosis
1. Compensated cirrhosis
- The disease may be discovered at a routine examination or biochemical screen.
- Cirrhosis may be suspected if the patient has fatigue (the most common and early symptom), mild pyrexia, vascular spiders, palmar erythema, or unexplained epistaxis or edema of the ankles.
- Firm hepatomegaly and splenomegaly are helpful diagnostic signs.
2. Decompensated cirrhosis
Cirrhotic patients are considered decompensated if they have developed ascites, variceal bleeding, jaundice, and or encephalopathy, The patient usually seeks medical advice because of ascites and/or jaundice, Ascites are usually manifested by abdominal distension.
General health fails with weakness, and muscle wasting (sarcopenia), which is associated with hepatic encephalopathy and prognosis of cirrhosis) and weight loss, Continuing mild fever (37.5-38C) is often due to Gram-negative bacteremia, Flappy tremors may be present due to hepatic encephalopathy.
Jaundice implies that liver cell destruction exceeds the capacity for regeneration and is always serious (marked decompensation), The skin may be pigmented due to defects in melanin metabolism, and Purpura over the arms, shoulders, and lower limbs may be associated with low platelets count.
Spontaneous bruising and epistaxis reflect a prothrombin deficiency, The circulation is overactive. The blood pressure is low, Sparse body hair, vascular spiders, palmar erythema, white nails, gonadal atrophy, and gynecomastia are common, Edema of the legs is frequently associated, The liver may be enlarged or shrunken, with a firm regular edge, The spleen may be palpable.
Assessment of severity of cirrhosis
- Child-Pugh scoring system for cirrhosis.
- Clinical types of cirrhosis.
Laboratory investigations
1. Hematology
- Anemia: There is usually mild normocytic, normochromic anemia; it is occasionally macrocytic, GI bleeding leads to hypochromic anemia.
- Leucopenia.
- Thrombocytopenia: once the platelet count reaches 100.000/uL that represents clinically significant portal hypertension.
- The prothrombin time is prolonged and does not return to normal with vitamin K therapy due to reduced synthesis of prothrombin by the liver.
2. Serum biochemical changes
- Serum bilirubin level may be raised.
- Serum albumin is decreased.
- Gamma globulin is raised.
- Serum phosphatase is usually raised.
- Serum transaminase values may be normal or raised (raised in case of an untreated virus or uncontrolled condition).
3. Liver Biopsy
May give a clue to the etiology and inflammatory activity. If there are contraindications, such as ascites or coagulation defects, the (trans-jugular approach should be used, Reticulin and collagen stains are essential for the demonstration of fibrosis around the nodules.
A liver biopsy is a gold standard for grading and staging disease, It is invasive, and expensive, Needle liver biopsy samples < 1/50,000th of the liver, and Incorrect staging of 1 stage in 10% to 20% of cases.
Dependent on:
- Length of biopsy -25 mm optimal (16%).
- The number of biopsies.
- Type of biopsy needle used.
- Etiology of liver disease.
4. Abdominal ultrasound
- Simple and non-invasive.
- Mixed echo pattern.
- Dilated portal vein: more than 13 mm.
- Enlarged spleen: more than 13 cm.
- Ascites.
Complications of cirrhosis
- Gastro-esophageal variceal bleeding or bleeding from portal gastropathy.
- Hepatic (Porto-systemic) encephalopathy.
- Ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome.
- Hepatocellular carcinoma.
- Cardiopulmonary complications.
Treatment of cirrhosis
The major goals of treating patients with cirrhosis include:
- Slowing or reversing the progression of liver disease.
- Preventing superimposed insults to the liver.
- Preventing and treating the complications (varices and ascites).
- Determining the appropriateness and optimal timing for liver transplantation.
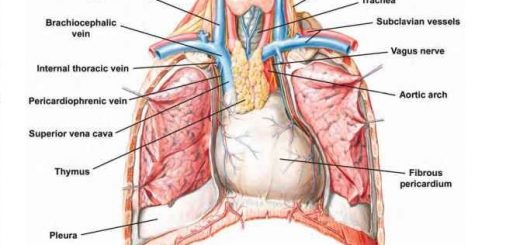
Portal Hypertension
Portal hypertension results from a combination of increased portal venous inflow and increased resistance to portal blood flow, Portal hypertension represents an increase in the hydrostatic pressure within the portal vein or its tributaries, Splenic pressure > 15 mmHg. Hepatic Venous Pressure Gradient HVPG > 5 mmHg, HVPG is measured by the catheterization of the hepatic vein (HVPG = Wedged hepatic venous pressure – IVC pressure) normally it is 5 mmHg or less.
Complications of portal hypertension begin to develop when HVPG reaches a value>10 mm Hg, (Clinically significant portal hypertension).
Pathophysiology of PHEN
1. Increased intrahepatic resistance
a) Architectural disturbances (mechanical components)
- Distortion of vascular architecture by fibrosis, scarring, regenerative nodules, and thrombosis.
- Fixed.
- 70%.
b) Functional alterations (dynamic component)
- Active contraction of hepatic stellate cells, vascular smooth cells in the portal venules & myofibroblasts.
- Modifiable by drugs.
- 30%.
c) Vasodilator/vasoconstrictor imbalance
- Increased (vasoconstrictor): Endothelin, angiotensin, norepinephrine, ADH, leukotrienes, thromboxane, and others.
- Decreased (Vasodilator): Nitric oxide (NO), carbon monoxide (CO) and others.
2. Increased blood flow
Due to splanchnic vasodilation
The basic treatment of PHTN
1. By decreasing hepatic resistance (mechanic/dynamic) by Vasodilators or TIPS
- Dynamic increased hepatic resistance is managed by vasodilators such as nitrate which sometime may not be effective inside the liver.
- TIPS is used in high pressure.
2. By decreasing splanchnic blood flow by Vasoconstrictors
- Terlipressin and somatostatin are used in acute cases.
- B blockers are used in chronic cases.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Gastro-esophageal varices cause, treatment, and therapy of variceal bleeding
Viral hepatitis, HDV symptoms, Treatment of acute HCV, Occult hepatitis C and HEV
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Portal Venous System, Histological structure of Liver, portal vein and its tributaries
Liver development, congenital anomalies, function & Pancreas development