Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
For any patient with liver failure, you must know whether he has normal liver or with liver cirrhosis. If you have a patient with acute liver failure you must specify whether acute on top of normal liver (acute liver failure) or acute on top of cirrhotic liver (acute on chronic liver failure).
Acute liver failure
Definition: A highly specific and rare syndrome, characterized by an acute deterioration of liver function without underlying chronic liver disease, Acute liver injury like acute hepatitis, most patients will recover spontaneously, However, some patients may pass into a more severe disease called Severe Acute Liver Injury.
Severe Acute Liver Injury + HE = ALF
Etiology
Drugs: Paracetamol, Anti-TB, chemotherapy, statins, NSAIDs, phenytoin, carbamazepine, ecstasy, and flucloxacillin.
Acetaminophen toxicity
Dose: Single dose > 15 gm in non-alcoholic or daily dose 3-8 gm. in alcoholic, malnourished patients.
Mechanism: acetaminophen is metabolized into a toxic intermediate metabolite (N-acetyle-P-benzoquinoneimine) which induces massive liver necrosis) and it is normally cleared by glutathione), The store of glutathione is decreased in alcoholic and malnourished patients. Therefore, the toxicity of Acetaminophen in alcoholic and malnourished patients may come in smaller doses.
Viral: Hepatitis B, A, E (especially in a pregnant woman), Less frequent CMV, HSV, VZV, Dengue.
Toxins: Amanita phalloides, phosphorus.
Vascular: Budd-Chiari syndrome, Hypoxic hepatitis (ischemic hepatitis).
Pregnancy: Pre-eclamptic liver rupture, HELLP, fatty liver of pregnancy.
Others: Wilson disease, autoimmune, lymphoma, malignancy HLH.
Classification
- Classification is according to the time interval between the jaundice as the first manifestation of acute liver injury to the occurrence of hepatic encephalopathy.
- The value of this classification: it’s important to build up our treatment plan and prognosis.
- Hyperacute and acute forms are usually associated with cerebral edema and carry better prognosis than other forms of liver failure.
- Therefore, you must concentrate on the management of brain edema in these patients.
- According to the duration of the interval between the onset of jaundice and the appearance of hepatic encephalopathy:
- Fulminant: duration is less than 2 weeks.
- Subfulminant: duration is more than 2 weeks and less than 12 weeks.
Another classification
- Hyperacute: duration is less than I week.
- Acute: duration is more than 1 week and less than 4 weeks.
- Subacute: duration is more than 4 weeks and less than 12 w.
- Chronic: duration is more than 12 w.
- Acute on chronic.
Fulminant and hyperacute forms primarily occur on top of the normal liver. They are usually associated with cerebral edema and carry a better prognosis than other forms of liver failure.
Clinical picture
The first 3 points are the main points for the diagnosis of acute liver failure:
- Jaundice: hepatocellular jaundice (the initial manifestation of acute liver disease).
- Coagulopathy: bleeding diathesis due to reduced PT and platelet count resulting in epistaxis, vaginal bleeding, hematemesis and/or melena.
- Hepatic encephalopathy (on top of no. 1 & 2).
- Ascites: usually mild and may be tense (may or may not happen) & occurrence of brain edema.
- Cerebral edema; (especially in the hyperacute and acute form).
- The commonest identifiable cause of death in FHF, You can diagnose brain edema by CT brain or MRI brain.
- Mechanism: vasogenic or cytotoxic theory leading to impaired cerebral blood flow and increased ICP leading to brain stem herniation and anoxic brain and may be irreversible neurological deficits.
Signs
- Hyperventilation, systemic hypertension,
- Abnormal pupillary reflexes.
- Muscle rigidity or decerebrate posture.
- Lately impaired brain stem functions and papilledema.
6. Fetor hepaticus
- The sweetish fecal odor of the smell is due to increase levels of methyl mercaptans which are normally detoxified by the liver.
- Significance: Sure sign of liver failure when the diagnosis is doubtful and carries a poor prognosis in FHF as it may precede the coma stage.
- However, in patients with chronic liver failure with acute on chronic it’s not of prognostic value.
- You may have a patient with fetor hepaticus without liver failure as it can occur in a patient with portosystemic collaterals without liver failure.
7. Renal failure
- Acetaminophen poisoning occurs early and is associated with a 95% mortality rate.
- In other cases occurs late and is associated with fluid retention (and maybe the occurrence of hepatorenal syndrome).
8. Respiratory failure
Due to ARDS (acute respiratory distress syndrome), pulmonary hemorrhage (hemorrhage within the alveoli).
9. Sepsis:
(bacterial and/or fungal infection (because they’re immunocompromised).
10. Metabolic disorders
- Hypoglycemia: multifactorial (the liver (hepatocyte) is responsible for glucose homeostasis).
- Acidosis: early and associated with poor prognosis in acetaminophen poisoning and late in other causes due to HRF.
- Alkalosis: due to hypokalemia.
- Hypoxemia: due to aspiration, atelectasis, infection, ARDS and pulmonary hemorrhage.
Lab Investigations
- Increased: S. bilirubin, Urea, and creatinine to know if the patient has associated renal failure and arterial blood ammonia.
- Decreased: PT, factor 5: decreased by > 50% normal S. albumin, S. Ca, Ph. Mg. K.
- AST, ALT: increased then decreased.
- ABG: acidosis or alkalosis.
Investigations to determine the cause of acute liver failure
- Toxicology screen of blood and urine.
- HBsAg, IgM anti-HBc.
- IgM anti-HAV.
- Anti-HEV, HCV, cytomegalovirus, herpes simplex, Epstein-Barr virus.
- Caeruloplasmin, serum copper, urinary copper, slit-lamp eye examination.
- Autoantibodies: ANA, ASMA, LKM, SLA.
- Immunoglobulins.
- Ultrasound of liver and Doppler of hepatic veins.
Management
- Exclude cirrhosis, alcoholic-induced liver injury, or malignant infiltration.
- initiate an early discussion with the tertiary liver/transplant centre (even if not immediately relevant).
- Screen intensively for hepatic encephalopathy.
- Determine etiology (to guide treatment and determine prognosis).
- Assess suitability for liver transplant (Contraindications should not preclude transfer to tertiary liver/transplant centre).
- Transfer to a specialized unit early (if the patient has an INR>1.5 and onset of hepatic encephalopathy or other poor prognostic features).
Nutrition: Enteral is better than parenteral feeding. Aggressively correct low levels of glucose, Ph, Ca, K, and Mg. Calories: 35-50 KCl/kg/d to meet the resting metabolic rate.
Correct coagulopathy: by vit K, FFP (fresh frozen plasma) and platelet.
Access for HE: and apply treatment Measures for HE.
Measures for brain edema: (you must search for and treat as early as possible especially in acute liver failure). Mannitol (standard treatment) till ICP decreases. Raise the head 10 degrees. Avoid hypoxia, and hypotension. Corticosteroids proved to be ineffective. (We don’t have to use them except if indicated like an acute autoimmune liver disease)
Anticipate and correct sepsis: by empirical or specific antibiotics.
Anticipate and correct renal failure: by fluids volume expanders dopamine ± hemodialysis.
Anticipate and correct respiratory failure & metabolic abnormalities.
In acetaminophen poisoning: N-acetyl cysteine I.V. infusion is used to restore glutathione stores (it has a Loading dose then a maintenance dose). It’s mainly used in a patient with acetaminophen poisoning. However, it can be used in other causes of acute liver failure, for example, alcoholic hepatitis)
Liver transplantation.
Acute on chronic liver failure (ACLF)
It is a clinical syndrome of acute hepatic decompensation observed in patients with pre-existing chronic liver disease and associated with one or more extrahepatic organ failures and increased mortality. Acute hepatic decompensation (defined as the acute development or worsening of ascites, overt encephalopathy, GI hemorrhage, non-obstructive jaundice and/or bacterial infections).
ACLF precipitating factors
Potential precipitating factor(s), either hepatic and/or extrahepatic. However, in a significant proportion of patients, a precipitant factor may not be identified.
Hepatic
- Heavy alcohol intake.
- Viral hepatitis.
- DILI (drug-induced liver injury).
- Autoimmune hepatitis.
Extrahepatic
- Infections.
- Hemodynamic derangements following hemorrhage.
- Surgery
ACLF grading
Grading ACLF helps clinicians assess the prognosis. ACLF is stratified into 3 grades based on its severity:
Grade-1 ACLF:
- Single renal failure.
- Single liver, coagulation, circulatory, or lung failure that is associated with a serum creatinine level of 1.5 to 1.9 mg/dL and/or hepatic encephalopathy grade 1 or grade 2.
- A single brain failure with a serum creatinine level of 1.5 to 1.9 mg/dl.
Grade-2 ACLF: It is diagnosed when there are 2 organ failures of any combination.
Grade-3 ACLF: It is diagnosed when there are 3 or more organ failures of any combination.
Management
Prevention of precipitating factors leading to acute hepatic decompensation, supportive care, and early initiation of specific therapy, prevention, and management of complications. It also includes determining the prognosis and the need for liver support including possible liver transplantation. All patients should be hospitalized preferably at a center that has facilities for liver transplantation.
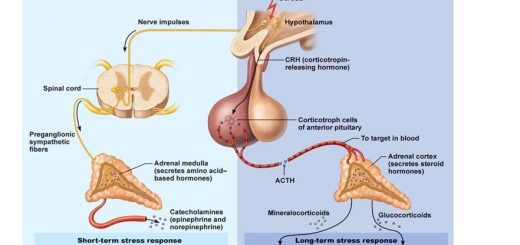
Hepatic encephalopathy
Pathogenesis of HE is multi-factorial, ammonia is the most important theory. The main stay of the treatment of HE is to Identify and correct the precipitating factor. Reduction of ammonia synthesis and absorption is the most important and approved step in the treatment of HE.
Liver failure
Liver failure could be acute or acute on chronic. Brain edema is the most common complication of acute liver failure. Treatment of liver failure should depend on the treatment of the cause and/or precipitating factors, anticipation and treatment of complications, and liver transplantation when needed.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Hepatorenal syndrome (HRS) risk factors, diagnosis, symptoms, types, causes and treatment
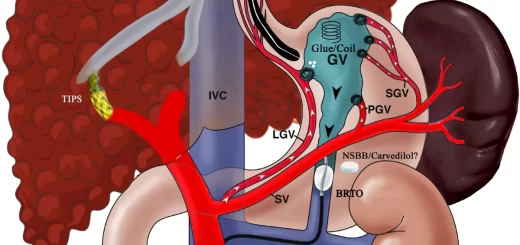
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Liver Cirrhosis causes, symptoms, treatment & stages, Liver Biopsy and treatment of PHTN
Viral hepatitis, HDV symptoms, Treatment of acute HCV, Occult hepatitis C and HEV
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Liver development, congenital anomalies, function & Pancreas development