Large intestine structure, function, Motility and Development of the digestive system
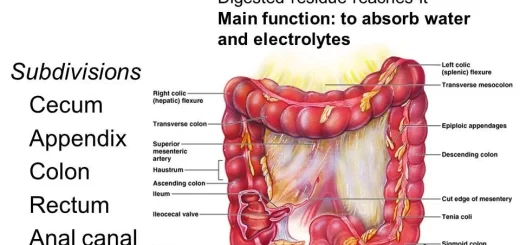
The large intestine is also known as the large bowel, It is the last part of the gastrointestinal tract and of the digestive system in tetrapods, It is the portion of the digestive system most responsible for absorption of water from the indigestible residue of food.
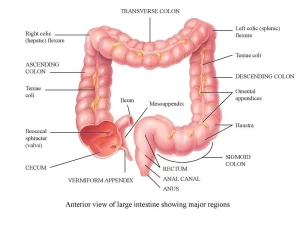
Large intestine
Physiologically, the large intestine could be divided into three parts:
- Proximal colon (for absorption), from the cecum to the middle of the transverse colon.
- The distal colon (for storage), from the middle of the transverse colon to the junction of the pelvic colon with the rectum.
- The rectum and anal canal (for defecation).
Functions of the large intestine
1. Digestion
The large intestine has no digestive functions in man. In herbivores, cellulose is hydrolyzed into glucose by the action of bacteria in the colon.
2. Absorption
About 1500 ml of fluid chyme passes daily from the ileocecal valve. The amount of fluid in feces per day is about 200ml. This indicates that about 1300 ml of water has been absorbed in the large intestine, especially in the caecum and ascending colon. The large intestine can absorb water, salts, glucose, and other crystal-loids, but with a much slower rate than the small intestine.
3. Secretion
The only significant secretion in the large intestine is mucus, its rate of secretion is regulated principally by direct stimulation of the goblet cells and by local enteric reflex to the goblet cells in the crypts of Lieberkuhn. Parasympathetic stimulation to the distal part of the large intestine causes a marked increase in mucus secretion.
Mucus has the following functions
- It protects the wall against mechanical and chemical irritation.
- It provides the binding medium for holding fecal matter together and lubricates the feces.
- It neutralizes the acids produced by bacterial fermentation, due to its alkaline reaction.
In addition to the mucus, the mucosa secretes large quantities of water and electrolytes in cases of bacterial infection, to dilute the irritating factors and to cause rapid movement of the feces toward the anus.
4. Actions of bacterial flora
In the large intestine, bacteria synthesize valuable substances such as vitamin K. vitamin B complex and some amino acids. These substances are absorbed and supplement the dietary vitamins. Prolonged use of antibiotics and intestinal antiseptics destroy the bacteria leading to vitamin deficiency.
5. Storage of feces
Feces are stored in the pelvic colon till the time of defecation.
6. Defecation
Innervation of the large intestinal muscles
1) Parasympathetic supply
The vagi supply the proximal colon with motor fibers, and the pelvic visceral nerve (Sacral 2, 3, 4) supplies the remaining part of the wall of the large intestine, but it is inhibitory to the internal anal sphincter. In general, the parasympathetic supply increases the tone and movements and helps the emptying of the large intestine and defecation.
2) Sympathetic supply
It arises from lumbar 1-4. It is inhibitory to the muscles of the entire colon, but it is excitatory to the internal anal sphincter.
3) Somatic supply
The external anal sphincter is supplied by the pudendal nerve from sacral 2-4. It is a voluntary muscle, Therefore is under voluntary, conscious, or at least subconscious control; subconsciously, the external sphincter is usually kept continuously constricted unless conscious signals inhibit the constriction.
Motility of the large intestine
The movements of the colon include segmentation contractions and peristaltic waves like those occurring in the small intestine, The third type of contraction that occurs only in the colon is the mass action contraction, in which there is a simultaneous contraction of the smooth muscle over large confluent areas, It is facilitated by the gastro-colic and duodeno-colic reflexes, These contractions propel the fecal material in one segment en masse further down the colon, They also move material into the rectum, causing rectal distension which initiates the defecation reflex.
Defecation
It is a complex muscular act to empty the colon from the middle of the transverse part to the anus.
The automatic spinal mechanism
1. Most of the time, the rectum is empty of feces. The ingestion of food and distension of the stomach and duodenum stimulates 2 reflexes; the gastrocolic reflex and duodeno-colic reflex. These 2 reflexes stimulate mass movement to push the contents of the pelvic colon into the rectum leading to its distension. The reflexes are transmitted by way of the autonomic nervous system.
2. Distension of the rectal wall initiates two defecation reflexes:
a- Intrinsic defecation reflex: which is mediated by the local enteric nervous system in the rectal wall as follows: Distention of the rectum stimulates afferent signals that spread through the myenteric plexus to initiate peristaltic waves in the descending colon, sigmoid, and rectum, forcing feces toward the anus.
As the peristaltic wave approaches the anus, the internal anal sphincter is relaxed by inhibitory signals from the myenteric plexus; if the external anal sphincter is relaxed at the same time, defecation occurs. This reflex by itself is relatively weak. To be effective in causing defecation, it usually must be fortified by the parasympathetic defecation reflex.
b- Parasympathetic defecation reflex that involves the sacral segments of the spinal cord. When the nerve endings in the rectum are stimulated, afferent signals are transmitted first into the spinal cord (along the pelvic nerve through the posterior roots of sacral segments 2, 3, 4) and then reflexly back to the descending colon, sigmoid, rectum, and anus by way of parasympathetic nerve fibers in the pelvic nerves again.
These parasympathetic signals greatly intensify the peristaltic waves and relax the internal anal sphincter, thus converting the intrinsic myenteric defecation reflex from a weak effort into a powerful process of defecation.
3. Defecation signals entering the spinal cord initiate other effects such as:
- taking a deep breath
- closure of the glottis
- contraction of abdominal wall muscles to force the colon contents downward.
- descent of the pelvic floor downward, thus straightening the anorectal angle to expel the feces.
Voluntary control of defecation
Distension of the rectum increases the rectal pressure and evokes afferent impulses to the visceral cortex. This leads to the sensation of desire for defecation. The conscious mind voluntarily controls the external anal sphincter, and either relaxes it to allow defecation to occur or further contracts it if it is not convenient for the person to defecate. In addition, voluntary straining contracts the diaphragm and muscles of the anterior abdominal wall. This increases the intra-abdominal pressure and helps empty the colon and rectum.
In newborn babies and in some people with transected spinal cords, the defecation reflexes cause automatic emptying of the lower bowel at inconvenient times during the day because of a lack of conscious control exercised through voluntary contraction or relaxation of the external anal sphincter. The frequent voluntary inhibition of the defecation reflex is the most common cause of constipation.
Development of the digestive system
Origin:
- The endoderm of gut (except mouth and lower half of anal canal which are ectodermal) → mucosa & its glands.
- Splanchnic secondary mesoderm → smooth muscles and connective tissue.
- It is formed from the incorporation of the dorsal part of the yolk sac into the embryo due to head, tail, and lateral folds.
- It extends from the oral membrane to the cloacal membrane.
Development of the primitive gut tube
The primitive gut tube extends from the oral membrane to the cloacal membrane, It is divided into:
- Foregut: from the pharynx to the middle of 2nd part of the duodenum.
- Midgut: from the lower half of 2nd part of the duodenum to the junction between right 2/3 & left 1/3 of the transverse colon.
- Hindgut: the remaining part of the large intestine.
Arterial supply of the gut
- The foregut derivatives are supplied by the coeliac trunk.
- The midgut derivatives are supplied by the superior mesenteric artery.
- The hindgut derivatives are supplied by the inferior mesenteric artery.
Development of the oesophagus
Origin:
- The endoderm of foregut → mucosa & its glands.
- Splanchnic secondary mesoderm → submucosa & musculosa.
- Mesenchyme of branchial arches → striated muscles of upper 1/3 of oesophagus.
Development
- The oesophagus at first is short then elongates.
- The trachea develops from its ventral border. They are communicating then a trachea-oesophageal septum develops between them.
- Epithelium of oesophagus proliferates, obliterating the lumen then recanalization occurs.
Congenital anomalies:
- Short oesophagus due to failure of elongation. It is associated with thoracic stomach
- Tracheo-oesophageal fistula: due to non-separation between trachea and oesophagus→ milk in lungs → pneumonia and air in stomach → respiratory distress.
- Oesophageal atresia: due to failure of recanalization. It is associated with poly hydroamnios.
- Oesophageal stenosis: due to incomplete recanalization.
Development of stomach
Origin:
- The endoderm of foregut → mucosa & its glands.
- Splanchnic secondary mesoderm→ submucosa, musculosa and serosa.
Development
Fusiform part of foregut
1- Its dorsal border grows more → greater curvature.
2- Its ventral border grows less → lesser curvature.
3- Most cranial part of the dorsal border grows rapidly → fundus.
Rotation of stomach 90° clockwise around its longitudinal axis→ Left surface becomes anterior & right surface becomes posterior. So left vagus becomes the anterior gastric nerve & right vagus becomes the posterior gastric nerve. The stomach was first vertical→ by the development of the liver →its long axis will be oblique.
4- Ventral mesogastrium → lesser omentum & falciform ligament.
Dorsal mesogastrium→ gastrosplenic, lienorenal ligament & greater omentum
Congenital anomalies:
- Thoracic stomach: associated with the short oesophagus.
- Congenital pyloric stenosis: due to hypertrophy of the circular muscles in the pyloric region→ projectile vomiting of the infant after feeding.
- Hourglass stomach.
- Transposition of the stomach (It may be associated with situs inversus).
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Small intestine constituents, Regulation, function & Digestion in the small intestine
Large Intestine function, parts, length, anatomy & Relations of the rectum
Stomach parts, function, curvatures, orifices, peritoneal connections & Venous drainage of Stomach
Pancreatic secretion composition, regulation, function, Differences between jejunum & ileum