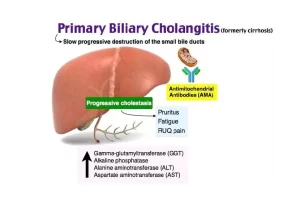
Primary biliary cirrhosis symptoms, cause, diagnosis, treatment, and Osteoporosis
Primary biliary cirrhosis is known as primary biliary cholangitis, It is a chronic disease in which the bile ducts in your liver are slowly destroyed, It mostly affects women, It is considered an autoimmune disease, which means your body’s immune system is mistakenly attacking healthy cells and tissue.
Epidemiology
- PBC is found in all races.
- Approximately 90-95% of patients are female.
- The age of onset typically ranges from 30 to 70.
- • It usually presents with a long-standing history of pruritis.
Immunologic abnormalities
A. Antimitochondrial antibody (AMA).
Detected in 95% of patients with PBC.
B. Increased levels of serum immunoglobulins (hyperglobulinemia)
Increased levels of a serum IgM that is immunoreactive and highly cryoprecipitate.
C. Association with other autoimmune diseases
- Thyroiditis, hypothyroidism.
- Rheumatoid arthritis.
- CREST syndrome (calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, telangiectasia).
- Sjögren’s syndrome.
- Scleroderma.
Pathogenesis
Two related processes cause hepatic damage in PBC:
The first process
Is the chronic destruction of small bile ducts, presumably mediated by activated cytotoxic T lymphocytes.
The second process
- Is chemical damage to hepatocytes in areas of the liver where bile drainage is impeded by the destruction of the small bile ducts.
- The destruction of bile ducts eventually leads to portal inflammation and scarring, and ultimately to cirrhosis and liver failure.
Hepatic histology
A. Stage I
- Damaged bile ducts are usually surrounded by a dense infiltrate of mononuclear cells, most of which are lymphocytes.
- Florid bile duct lesion.
- The epithelial cell lining of a duct is infiltrated with lymphocytes.
- This leads to inflammation and obliteration.
B. Stage II
- The lesion is more widespread.
- There may be reduced numbers of normal bile ducts within portal triads and increased numbers of atypical, Poorly formed bile ducts with lucia irregularly shaped lumina.
- There is diffuse portal fibrosis and mononuclear cell infiltrates within triads.
- Inflammation may spill into the surrounding periportal areas.
- A typical bile duct hyperplasia.
- There are tortuous bile ducts with inflammatory cell infiltration consisting of primarily lymphocytes and few neutrophils.
C. Stage III
- Similar to stage II except that fibrous septa extend beyond triads and from portal to portal bridges.
- Portal to the portal fibrous septum is shown (Masson trichrome).
- It reached cirrhosis (cirrhotic nodules).
D. Stage IV
- Represents the end stage of the lesion, with frank cirrhosis and regenerative nodules.
- The findings may be indistinguishable from other types of cirrhosis.
- However, a paucity of normal bile ducts in areas of scarring suggests the possibility of PBC.
- There is a noncaseating granuloma in the center of and portal trials are linked by bands of connective tissue and inflammatory cells. (Masson trichrome).
- The bile duct is completely obliterated so there will be no bile secretion and bile stasis which is toxic to the hepatocytes, undergoes the process of necrosis regeneration and cirrhotic nodules with extensive large formation of cirrhotic nodules.
Clinical features
About 48-60% of patients are asymptomatic at the time of diagnosis. The symptoms and signs of PBC are due to long-standing cholestasis:
- Fatigue: Most common symptom.
- Pruritus: The earliest specific complaint of PBC is pruritus.
- Malabsorption: Impaired secretion of bile leads to malabsorption of the fat-soluble vitamins A, D, E, and K, and calcium.
Osteoporosis
- The osteopenic bone disease occurs in at least 25% of PBC patients. The pathogenesis is still unclear.
- Osteomalacia is uncommon and occurs only in home-bound patients who have advanced PBC and little exposure to sunlight.
Physical examination
- Hepatomegaly is found in approximately 43-70% of patients.
- Splenomegaly is present 16-35%.
- Eves: Kayser-Fleischer rings are rare and result from copper retention.
- Skin abnormalities:
- The hyperpigmentation that resembles tanning is due to melanin, not bilirubin, in early-stage PBC.
- Excoriations may be diffuse due to scratching caused by intractable pruritus.
- Jaundice usually presents later in the course of the disease.
- Xanthelasma and xanthomata correlate with hypercholesterolemia.
- Less than 5% of patients will eventually develop xanthomata.
- Xanthomata are found on the palms of the hands and soles of the feet, over extensor surfaces of the elbows and knees, in tendons of the ankles and wrists, and on the buttocks.
Treatment
UDCA (Ursodeoxycholic acid) and liver transplantation.
You can subscribe to science online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Diagnosis of the cause of jaundice, Hepatobiliary imaging, treatment of cholestasis and Pruritus
Liver Cholestasis types, causes, features, symptoms, diagnosis, and treatment
Conjugated hyperbilirubinemia cause, symptoms and treatment
Unconjugated hyperbilirubinemia causes, symptoms, diagnosis and treatment
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer
Interventional radiology types, Robotic endovascular systems advantages & disadvantages