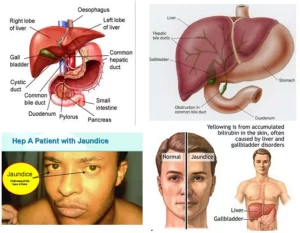
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Jaundice is also known as icterus, It is a yellowish or greenish pigmentation of the skin and sclera due to high bilirubin levels, Jaundice in adults is a sign indicating the presence of underlying diseases involving abnormal heme metabolism, liver dysfunction, or biliary-tract obstruction, The prevalence of jaundice in adults is rare, while jaundice in babies is common.
Jaundice
It is a condition in which the skin, whites of the eyes, and mucous membranes turn yellow because of a high level of bilirubin, a yellow-orange bile pigment, causes of Jaundice are hepatitis, gallstones, and tumors, In adults, jaundice usually doesn’t need to be treated.
The term jaundice denotes Yellowness that is seen in the sclera, skin, and mucous membranes when circulating bilirubin levels rise approximately 3-fold or more above normal, i.e., when serum bilirubin levels exceed about 3 mg/dL (51 μmol/L).
What is the source of bilirubin?
RBCs when they pass 120 days, they’re destructed in the RES including the liver and spleen releasing hemoglobin, Globin is a protein used in the re-synthesis of the RBCs.
Heme, the iron atom-containing heterocyclic tetrapyrrole ring. ferroprotoporphyrin IX, is catalytically cleaved to the water-soluble linear tetrapyrrole biliverdin, by microsomal heme oxygenase that oxidizes and opens the alpha-carbon bridge with the loss of iron and carbon monoxide.
Biliverdin is responsible for the green color in obstructive jaundice. The green pigment biliverdin is reduced by cytosolic biliverdin reductase to generate 250-400 mg of water-insoluble orange-yellow bilirubin each day. Biliverdin is converted to unconjugated Bilirubin by Biliverdin reductase.
Unconjugated Bilirubin has special features: Water Insoluble (it doesn’t filter through the kidney, and Lipophilic (it crosses the blood–brain barrier). Unconjugated Bilirubin moves in the blood bound to albumin until it reaches the liver.
In the liver sinusoids, bilirubin dissociates from albumin, to be taken up at the hepatocyte sinusoidal (basolateral) plasma membrane, probably by carrier-mediated facilitated diffusion, although the role of the organic anion transporting polypeptide 2 (OATP2), the proposed membrane carrier protein; is controversial. If this carrier (OATP2) is not available, this disorder is called Gilbert disorder).
Unconjugated Bilirubin enters the hepatocyte, it isn’t free in the cytoplasm, it’s bound to glutathione-S-transferases (originally identified as the aminoazodye-binding protein, ligandin Z and Y) and probably to some extent to fatty acid-binding protein too, so that bilirubin reflux back into the blood is retarded.
The obstacle to bilirubin elimination from the body via aqueous secretions, such as bile and urine, is overcome by conjugation in the liver with glucuronic acid, which converts bilirubin to its water-soluble glucuronides. The rate-determining step in the conjugation of bilirubin is the uptake of unconjugated bilirubin into the hepatocytes from sinusoidal blood.
Conjugation of bilirubin is a two-stage sequential reaction that takes place in the endoplasmic reticulum and is mediated by the bilirubin-specific isoform of uridine diphosphoglucuronosyl transferase (UGT) family of enzymes that uses uridine diphosphoglucuronic acid (UDPGA) to form bilirubin monoglucuronide first, and then the major conjugate, bilirubin diglucuronide.
Conjugated bilirubin is secreted into bile by an ATP-dependent active transport mechanism, which is mediated by the canalicular isoform of the multidrug resistance-associated Protein 2 (MRP2), which is also known as the canalicular multi-specific organic anion transporter (cMOAT).
If this pump is defective, we get a disorder called Dupin-Johnson. Bile flows from the canaliculi into the ducts of Hering, to the bile ductules (cholangioles), intralobular (terminal) bile ducts, and conducting area and segmental bile ducts.
Conjugated bilirubin is hydrolysed and reduced by bacterial beta-glucuronidase to urobilinogen Urobilinogen part of it is reabsorbed into the portal circulation and is re-excreted by the liver (called enterohepatic circulation), another part is secreted via the kidney and this is the source of Urobilinogen in urine in case of complete obstruction of the bile duct, there’ll be no urobilinogen in the urine. Urobilinogen undergoes further Oxidation into Urobilin which is responsible for the brown color of stool.
Bilirubin is the end-product of the degradation of heme:
- 80% comes from senescent red cell hemoglobin.
- 20% is derived from the turnover of other hemoproteins as;
- Myoglobin.
- Tissue mitochondrial.
- Microsomal cytochromes; catalase, peroxidase, and tryptophan pyrrolase.
Clinical classification of jaundice
- Pre-hepatic: The pathology is occurring prior to the liver.
- Hepatic: The pathology is located within the liver.
- Post-Hepatic: The pathology is located after the conjugation of bilirubin in the liver. (The bile ducts until they enter into the duodenum).
Classification of hyperbilirubinemia
- Unconjugated hyperbilirubinemia.
- Conjugated hyperbilirubinemia.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Hepatocellular carcinoma symptoms, stages, risk factors, diagnosis, and treatment
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Hepatorenal syndrome (HRS) risk factors, diagnosis, symptoms, types, causes, and treatment
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer
Common procedures of Interventional Radiology and the best Interventional Radiologists
Interventional radiology types, Robotic endovascular systems advantages & disadvantages