Acute HBV treatment, chronic HBV symptoms, Source of hepatitis B infection and risk of chronic infection
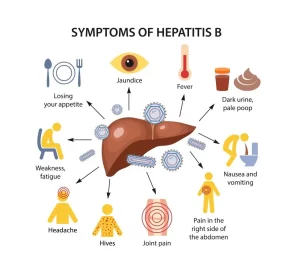
Acute hepatitis B takes place within the first 6 months after someone is exposed to the hepatitis B virus, Some people with acute hepatitis B have no symptoms at all or only mild illness, acute hepatitis B can cause a more severe illness that requires hospitalization, Hepatitis B infection causes a wide spectrum of liver diseases, from a subclinical carrier state to severe hepatitis or acute liver failure, particularly in older people, in whom mortality can reach 10 to 15%.
Acute HBV
- Incubation period 1 to 4 months.
- Bloodborne infection.
- Approximately 70% of patients have subclinical or anicteric hepatitis and only 30% have icteric hepatitis.
- During the prodromal period, a serum sickness-like syndrome manifesting as fever, skin rash, and arthralgia may develop.
- Less than 1% of patients with acute hepatitis B develop acute liver failure.
- There are seven markers related to hepatitis B: HBsAg – HBsAb- HBeAg – HBeAb -the anti-HB antibody IgM and IgG – HBV DNA polymerase.
Treatment of Acute HBV
- Symptomatic & supportive.
- Antiviral treatment (lamivudine in double dose, entecavir, Tenofovir) in severe acute HB only. If you start antiviral treatment in a patient with acute hepatitis B which is not severe you might precipitate chronicity.
- Characteristics of severe acute hepatitis B:
- Coagulopathy (INR > 1.5).
- Protracted course (persistent symptoms or marked jaundice for > 4 weeks.
- Signs of acute liver failure.
CHB
- About 90% of acute infections in infants become chronic.
- About 10% of acute infections in adults become chronic.
- HBeAg may transform into HBeAb so there are two forms of chronic hepatitis B: HBeAg-positive chronic hepatitis B and HBeAb-negative chronic hepatitis B. And in both, we find that: HBSA is positive, IgG anti-HBC and IgM anti-HBc is negative because it is a marker of acute infection not chronic.
Extrahepatic manifestations
- Polyarteritis nodosa.
- Glomerulonephritis.
- Essential mixed cryoglobulinemia.
- Guillain-Barre syndrome.
Treatment of chronic HBV
- 1st line drugs entecavir peg interferon alfa-2a and Tenofovir because of their superior efficacy, tolerability, and favorable resistance profiles.
- TAF has a lower dose than tenofovir and so has less toxicity.
- These drugs are planned to be taken lifelong except interferons which are taken for only one year so we must ensure that the virus won’t acquire resistance against drugs easily.
Occult HBV (form of chronic hepatitis B)
- The detection of HBV DNA in the absence of HBsAg.
- HBV DNA is detected in the liver in most cases, but is undetectable or present at low concentrations in the serum.
- Anti-HBc Abs are usually +ve.
- More common among patients with cirrhosis or HCC, Many of these patients probably had chronic HBV infection for decades, leading to liver damage, but HBsAg is no longer detectable when cirrhosis or HCC is diagnosed.
- HBsAg which the marker of chronic hepatitis is negative is why they are turned to occult HBV.
Post-exposure prophylaxis
Vaccinated:
- Anti HBs Ab > 10 mIU/ml no treatment.
- Anti HBs Ab < 10 mIU/mlIBIG + booster dose.
Not vaccinated:
- HBs Ag, anti HBc Ab, anti HBs Ab.
- Anti HBs Ab> 10 mIU/ml no treatment.
- Anti HBs Ab < 10 mIU/ml HBIG + vaccinate.
Vaccination should be provided as soon as possible, not later than seven days, After exposure; HBIG should be administered not later than within 72 hours, Test HBV infection markers (HBsAg, anti-HBc IgM) at 6, 12 and 24 weeks post-exposure.
Vertical transmission might occur in HBV from the mother to infants during delivery and these neonates when acquiring this infection at this age, 90% of these cases may be chronic and may have complications of cirrhosis at the age of 20-30 years. And to protect neonates from this infection we must:
- Decrease the viral load in the mother in the last 3 months of pregnancy.
- Give neonates HBIG and start vaccination.
Source of hepatitis B infection and risk of chronic infection
Horizontal transmission (10%)
- Injection drug use.
- Infected unscreened blood products.
- Tattoos/acupuncture needles.
- Sexual transmission.
- Close living quarters/playground play as a toddler (may contribute to a high rate of horizontal transmission in Africa).
Vertical transmission (90%)
Hepatitis B surface antigen (HBsAg)-positive mother.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Histological structure of gallbladder & Pancreas, Functions of the liver & Composition of bile
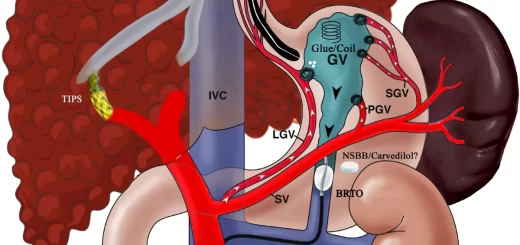
Portal Venous System, Histological structure of Liver, portal vein and its tributaries
Histology of pancreas, Structure of islets of Langerhans, Insulin function & Metabolism
Liver development, congenital anomalies, function & Pancreas development