Antibacterial agents types, Effect of Antibacterial Drugs and How do antibiotics work?
Antibacterial agents are a group of materials that fight against pathogenic bacteria, so, by killing or reducing the metabolic activity of bacteria, their pathogenic effect in the biological environments will be minimized. Antimicrobial agents can prevent bacterial plaque accumulation in the oral environment and therefore, they can reduce the prevalence of plaque-related diseases such as caries.
Antibacterial agents
Antimicrobial agents are a large variety of chemical compounds and physical agents that are used to destroy microorganisms or prevent their development.
Classification of antibacterial agents
Classification of antibacterial agents may be based on their spectrum and mechanisms of action.
The spectrum of activity of antibacterial agents
a- Narrow spectrum, acting mainly against selected bacteria:
- Antibiotics acting mainly against Gram-positive organisms e.g. benzyl penicillin (penicillin G) and vancomycin.
- Antibiotics acting mainly against Gram-negative organisms e.g. polymyxins, aztreonam, and aminoglycosides.
b- Broad-spectrum, Antibiotics are acting against both Gram-positive and Gram-negative bacteria e.g. sulphonamides-trimethoprim, tetracyclines, chloramphenicol, fluorinated quinolones (norfloxacin, ciprofloxacin, pefloxacin), ampicillin and Amoxycillin.
Bacteriostatic antibiotics: are capable of inhibiting the growth or reproduction of bacteria as tetracyclines. Bactericidal antibiotics are capable of killing bacteria such as penicillins.
Selective toxicity. The antibiotic selectively inhibits or kills the microorganism but has little or no toxic effect on the patient. It is accomplished by finding vulnerable targets in the microbe (e.g. bacterial cell wall) that do not exist in the human host. It may also depend on the inhibition of biochemical events essential to the pathogen but not to the host (e g cotrimoxazole).
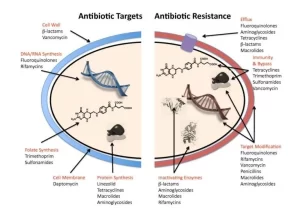
Mechanisms action of antibacterial drugs
It is convenient to present these mechanisms of action under 6 headings:
Antibacterial action through inhibition of cell wall synthesis
(All penicillins, all cephalosporins, carbapenems, monobactams, and glycopeptides). These drugs are selective inhibitors of bacterial cell wall synthesis All are bactericidal agents. It is important to remember that all antibiotics inhibiting cell wall synthesis are effective only on growing cells (metabolically active cells).
Penicillins
They are B-lactam drugs that bind to cell wall receptors called penicillin-binding proteins (PBPS), some of which are (transpeptidases that catalyze the final cross-linking step in the synthesis of peptidoglycan. After a β-lactam drug has attached to its receptors, the transpeptidation reaction (cross linking) is inhibited and peptidoglycan synthesis is blocked, A final bactericidal event is the activation of autolytic enzymes in the cell wall resulting in cell lysis.
They are more during the log phase of bacterial cell growth. They are activated by β-lactamases that cleave the β-lactam ring.
Cephalosporins
They are β-lactam drugs that act in the same manner as penicillins.
Carbapenems
They are broad-spectrum β-lactam drugs that are structurally different from penicillins and cephalosporines and they are not inactivated by β-lactamases, however, carbapenemases that degrade them have recently emerged.
Monobactams
They are narrow spectrum β-lactam drugs that are structurally different from penicillins and cephalosporines and they are not inactivated by β-lactamases. The first marked monobactam was aztreonam.
Glycopeptides
A glycopeptide is not a β-lactam drug and it is not inactivated by β-lactamases. These antimicrobial drugs, acting on both aerobic and anaerobic Gram-positive organisms that inhibit peptidoglycan synthesis by binding to the specific precursors of the cell wall thus preventing it from accomplishing its action (β-lactam drugs bind to the transpeptidase itself), e.g. vancomycin & teicoplanin. Relative to other antibiotics, they are extremely large which prevents them from passing through porins in the outer membrane of Gram-negative bacteria.
Antibacterial action through inhibition of cell membrane function
The cytoplasmic membrane of bacteria is structurally and chemically similar to that of human cells, Consequently, it is difficult to obtain an antibiotic with sufficient selective toxicity. One advantage of antibiotics that affect bacterial cell membranes is that they are lethal (bactericidal) even to non-growing cells. Examples include; the polymyxins [e.g. polymyxin E (Colistin) acting on many resistant Gram-negative rods. They disrupt the phospholipid structure of the cell membrane.
Antibacterial action through inhibition of protein synthesis
Bacteria have 70 S ribosomes, whereas mammalian cells have 80 S ribosomes The subunits of each type of ribosome, and their chemical composition is sufficiently different to explain why antimicrobial drugs can inhibit protein synthesis in bacterial ribosomes without having a major effect on mammalian ribosomes, The antimicrobial drugs inhibit protein synthesis either by acting on the 30 S subunit or the 50 S subunit.
Drugs acting on the 30 Subunit include:
- Aminoglycosides (eg Gentamicin, Streptomycin, Tobramycin, Amikacin). The effect of aminoglycoside is bactericidal, especially against Gram-negative rods.
- Tetracyclines which are bacteriostatic drugs. They are broad-spectrum antibiotics, Their selectivity is based on their increased uptake by susceptible bacterial cells compared with human cells (so they become more concentrated inside bacterial cells).
- Glycylcyclines e.g. tigecycline, they are similar to tetracyclines in almost all aspects. However, alterations of the molecule resulted in its expanded spectrum of activity and decreased susceptibility to the development of resistance when compared with other tetracycline antibiotics.
Drugs acting on the 50 S subunit include:
Chloramphenicol, Macrolides, Clindamycin, Linezolid, and Streptogramins.
- Chloramphenicol: It has a broad-spectrum bacteriostatic activity. However, it is rarely used due to its serious side effects.
- Macrolides (e.g. erythromycin, oleandomycin, clarithromycin, and azithromycin): They are bacteriostatic drugs with a wide range of activity especially, the new ones e.g. azithromycin.
- Clindamycin: It is a bacteriostatic drug which is mostly active against Gram-positive organisms and anaerobes.
- Linezolid: It is a bacteriostatic drug. It is useful in the treatment of many antibiotic-resistant Gram-positive bacteria e.g. vancomycin-resistant enterococci, mathicillin-resistant Staphylococcus aureus, and penicillin-resistant pneumococci.
- Streptogramins (Quinopristin/dalfopristin): These two agents act synergistically to achieve bactericidal activity against antibiotic-resistant Gram-positive bacteria not seen with either agent alone.
Antibacterial action through inhibition of nucleic acid synthesis
- Rifampin: It blocks mRNA synthesis by inhibiting bacterial RNA polymerase. Thus, it inhibits bacterial RNA synthesis. Rifampin has no effect on the RNA polymerases of mammalian cells, Rifampin is given in combination with other drugs because resistant mutants appear at a high rate when it is used alone, Such combinations are used in the treatment of serious infections like tuberculosis and prosthetic-valve endocarditis.
- Quinolones (e.g.ciprofloxacin, ofloxacin, levofloxacin, moxifloxacin): They are broad-spectrum bactericidal drugs active against many Gram-positive and Gram-negative bacteria. They inhibit bacterial DNA synthesis by blocking the DNA gyrase.
Antibacterial action through inhibition of bacterial metabolism
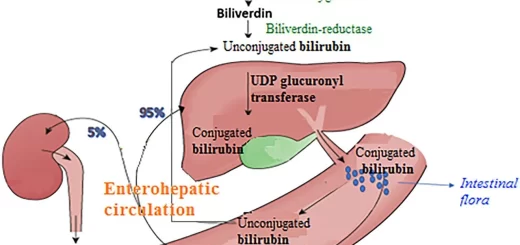
Sulfonamides: P-amino benzoic acid (PABA) is an essential metabolite, it is used by bacteria as a precursor in the synthesis of folic acid, which serves as an important step in the synthesis of nucleic acids, Sulfonamides are structural analogues of PABA and inhibit dihydrofolic acid synthetase.
They can enter the reaction in place of PABA and compete for the active center of the enzyme. As a result folic acid is not formed, preventing the further growth of bacterial cells Inhibition by sulfonamides is selective (i.e. toxic only to bacterial cells) because animal cells can’t synthesize folic acid and must depend upon exogenous sources.
Trimethoprim inhibits dihydrofolic and reductase 50 000 times more efficiently in bacteria than in mammalian cells, This enzyme reduces dihydrofolic to tetrahydrofolic acid a stage leading to the synthesis of purines and ultimately of DNA, If sulfonamides and trimethoprim are used together, they produce sequential blocking resulting in a marked enhancement (synergism) of activity. The combination is called cotrimoxazole, It consists of 5 parts sulfonamides plus one-part trimethoprim.
Miscellaneous antibacterial agents
Isoniazid is a bactericidal drug acting against Mycobacterium tuberculosis and other mycobacteria, It inhibits mycotic acid synthesis which explains why it is specific for mycobacteria and relatively nontoxic for humans.
Ethambutol is a bacteriostatic drug acting against Mycobacterium tuberculosis and many of the atypical mycobacteria. It inhibits the synthesis of arabinogalactan which inks mycolic acid with peptidoglycan.
Pyrazinamide is a bactericidal drug acting against Mycobacterium tuberculose but not against the atypical ones. It is particularly effective against the latent organisms in the lesion which are not affected by other antituberculous drugs.
Metronidazole is an antiprotozoal drug but has activity against anaerobic bacteria. It inhibits DNA synthesis.
Probiotics: These are not chemical antibiotics. but they are five non-pathogenic bacteria that may be effective in the treatment or prevention of certain human diseases. They bind to the receptor sites on the mucosa thus preventing the pathogenic bacteria from exerting their harmful effect i.e. they cause colonization resistance by which the non-pathogen excludes the pathogen from binding to its target site. Some of the best evidence in support of probiotic health benefits is in the treatment of antibiotic-associated diarrhea by Lactobacillus mamnosus.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Microbiology, Bacteria structure, types, Gram-positive bacteria & Gram-negative bacteria