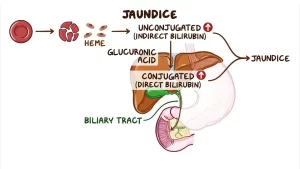
Unconjugated hyperbilirubinemia causes, symptoms, diagnosis and treatment
In unconjugated hyperbilirubinemia, elevated serum or plasma bilirubin levels are above the reference range of the laboratory, Unconjugated hyperbilirubinemia is due to dysregulation in the bilirubin metabolism that includes increased production, impaired hepatic uptake, and decreased conjugation of bilirubin, In newborns, unconjugated hyperbilirubinemia is very common, and increased bilirubin levels can cause life-threatening kernicterus.
Unconjugated hyperbilirubinemia causes
1. Bilirubin overproduction
- Excessive red cell breakdown (hemolysis (hematomas, etc.).
- Ineffective erythropoiesis (dyserytheropoiesis).
- Jaundice from pulmonary infarction or repeated blood transfusion.
2. Diminished bilirubin uptake by hepatocytes
Gilbert-Meulengracht syndrome.
3. Dysfunction of Bilirubin conjugation
Conjugation defect in which the conjugating enzymes have disorders, the conjugating enzymes which bind with Unconjugated bilirubin with glucuronic acid have a defect.
Physiologic jaundice of the newborn
- In about 90% of neonates, jaundice occurs 2-5 days of life and rarely exceeds 6 mg/dl.
- this is due to the immaturity of the conjugating enzyme (still inactive).
- The disorder is due to:
- Short erythrocyte life span (70-90) days.
- Reduction in cellular transport proteins.
- Difficeing in glucuronyl transferase.
- Increasing intestinal absorption of meconium bilirubin.
Breast milk jaundice
Possibly due to long-chain fatty acids in milk that inhibit uridine diphosphoglucuronyl transferase (the conjugating enzyme). It occurs in the first 2 weeks of life. Bilirubin level may reach up to 25 mg/dl and does not lead to kernicterus.
Lucy Driscoll syndrome
It is familial hyperbilirubinemia possibly due to the inhibitory effect of progestogen steroids in material blood which impedes bilirubin conjugation. Babies show sucking weakness, Jaudices start from the second day of life and regress after 2-3 weeks. The prognosis is good & in severe cases exchange blood transfusion may be required.
Gilbert’s syndrome
It’s a common disorder in which there’s a defect in the bump that transfers unconjugated bilirubin from the blood to inside the hepatocyte. It is a benign autosomal dominant partial defect of bilirubin conjugation Affecting 5-12% of the population. The disorder is 4 times more common in men than in women.
Pathogenesis: by several mechanisms:
- Elevated production of hepatic haembilirubin.
- Minor hemolysis.
- Reduced activity of Glucuronyl transferase.
- Disorders in the membrane fluidity are responsible for reduced bilirubin uptake by hepatocytes.
Clinical picture
Age of onset is between 15-30 years, there is intermittent unconjugated hyperbilirubinemia with bilirubin levels between 1.5 to 2.5mg/dl. The patient is asymptomatic or shows irritability, moodiness, and fatigue. (Due to worrying about hyperbilirubinemia).
Diagnosis
- Normal transaminase level.
- Regular ultrasound (liver is completely normal).
- Elevated level of unconjugated serum bilirubin.
Laboratory tests
- Increase in bilirubin on fasting and fall on taking Phenobarbital.
- The monoglucuronide/diglucuronide quotient is elevated.
- A fat-free diet for 3 days can cause bilirubin to double.
- Vigorous exercise for 1-2 days results in increased bilirubin levels.
- A nicotine acid test (50 mg nicotine acid I.V.) produces a rise in bilirubin of more than 0.9mg/dl.
Histology
- The liver is normal.
- Accumulation of the interlobular bile ducts and there may be a centroacinar deposit of higher amounts of lipofuscin.
- Gilbert has a normal life expectancy and reassurance is the only treatment required (no treatment is required).
- In severe cases administration of Phenobarbital of 80-160 mg/day.
Crigler-Najjar syndrome
1. Type I:
It is a hereditary recessive syndrome, there is a total lack of UDP glucuronosyltransferase due to gene mutation on chromosome no.2. Bilirubin excretion is reduced to 1-2% of the standard rate. Bilirubin may reach up to 50 mg/dl in the 1st days of life and kernicterus may develop.
It’s a life-threatening situation and leads to marked elevation of unconjugated bilirubin leading to kernicterus in which the unconjugated bilirubin crosses the blood-brain barrier and damages the brain, It’s fatal unless liver transplantation is done.
Therapy: Exchange blood transfusion/ phototherapy/cholestyramine/liver transplantation.
2. Type II:
It is a heterozygous defect where the glucuronosyltransferase activity is reduced. Bilirubin conjugation is minimally restricted. Jaundice may occur in the first year of life or during the next 20-30 years, Bilirubin fluctuates between 6-20mg/dl, Stressful factors increase bilirubin levels. Histology displays biliary thrombi and hypertrophy of the endoplasmic reticulum, Prognosis is good but repeated kernicterus may lead to permanent neurological damage.
Therapy:
- Phenobarbital 60 mg 3 times daily + calcium phosphate (Phenobarbital enhances biliary secretion of bile).
- Phototherapy with albumin infusion.
Kernicterus
It occurs because of the immaturity of the blood-brain barrier, in severe neonatal icterus and also in premature babies with bilirubin level higher than 20 mg/dl. Unconjugated bilirubin is deposited in the basal ganglia of the hippocampus and hypothalamus as bilirubin phosphatidylcholine which leads to neural necrosis hypothermia, hypoglycemia, and sepsis. In clinical terms, sucking weakness, vomiting, attacks of fever, convulsions, cramps, and nystagmus.
Therapy: Exchange blood transfusions, plasmapheresis, and phototherapy.
You can subscribe to Science Online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Conjugated hyperbilirubinemia cause, symptoms and treatment
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Hepatocellular carcinoma symptoms, stages, risk factors, diagnosis, and treatment
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Hepatic Artery Embolization, Importance and risks of Embolization therapy for Liver cancer
Common procedures of Interventional Radiology and the best Interventional Radiologists
Interventional radiology types, Robotic endovascular systems advantages & disadvantages