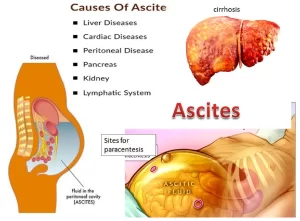
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Cirrhosis of the liver and different types of cancer can cause Ascites, fluid collects in spaces within your abdomen, when severe, ascites may be painful, The problem may keep you from moving around comfortably, symptoms of ascites: Swelling in the abdomen, Weight gain, Sense of fullness, Bloating, Sense of heaviness, Nausea or indigestion, Vomiting, Swelling in the lower legs, Shortness of breath, and Hemorrhoids.
Ascites
Ascites is an accumulation of free sterile fluid within the peritoneal cavity. Ascites forms because of conditions directly involving the peritoneum and diseases remote from the peritoneum.
Causes of ascites
A. Ascites with normal peritoneum
- Portal hypertension: Portal vein thrombosis, Liver cirrhosis, Veno-occlusive disease, Budd-Chiari syndrome, and IVC thrombosis.
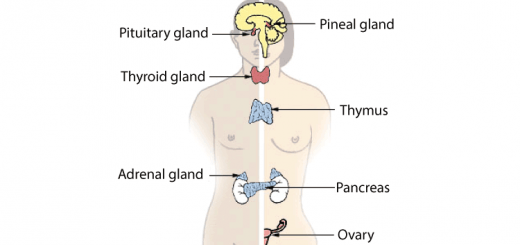
- Endocrine disease: Marked Hypothyroidism, Meig’s syndrome, Ovarian hyperstimulation, and Struma ovarii.
- Miscellaneous conditions: Chylous ascites, Bile ascites, Nephrogenic ascites, and Urine ascites.
- Cardiac diseases: Right heart failure, Constrictive pericarditis.
- Pancreatic disease: Acute pancreatitis, and Pancreatic pseudocyst.
- Hypoproteinemia: Nephrotic syndrome, Protein-losing enteropathy, Severe malnutrition.
B. Ascites with diseased peritoneum
- Infections: Tuberculosis, Fitz-Hugh-Curtis syndrome (chlamydiae, gonococci), Fungal (Coccidioidomycosis), HIV-associated peritonitis, Whipple’s Disease.
- Malignant ascites: Primary mesothelioma, Pseudomyxoma peritonei, Hepatocellular carcinoma, Massive hepatic metastases, Intraabdominal tumors.
- Other rare conditions: Familial Mediterranean Fever, Collagen Vascular Disease, Granulomatous peritonitis.
Pathophysiology of ascites
Mechanical factors
- Increase in hydrostatic pressure: Portal hypertension, Narrowing of IVC at the level of the diaphragm. Block of the hepatic veins.
- Reduction in colloid osmotic pressure.
- Disturbance of capillary permeability.
- Lymphatic circulation: Increased lymph formation, Insufficiency of lymphatic drainage.
Biochemical factors (renal sodium retention)
Increasing of:
- Renin-angiotensin-aldosterone.
- Antidiuretic hormone (ADH).
- Prostaglandins (Thromboxane).
- Endothelin.
- Catecholamines.
- Endotoxinaemia.
Decreasing of:
- Prostaglandins.
- (Prostaglandin E2 & Prostacyclin).
- Natriuretic factors (Atrial, Renal).
- Kallikrein-kinin system.
Pathophysiology of ascites formation in cirrhosis
- Approximately 60% of patients with compensated cirrhosis develop ascites during 10 years.
- The pathophysiology underlying the formation of ascites in cirrhosis is complex.
- There are many neurohormonal, renal, and systemic vascular abnormalities.
- Ascites is rarely due to portal hypertension alone (Localization factor).
- The triggering factor of ascites formation in cirrhosis is the accumulation of endogenous vasodilators such as nitric oxide, carbon monoxide, glucagon, peptides, and others, leading to peripheral and splanchnic arterial vasodilatation and underfilling of circulatory volume.
- This triggers the baroreceptor-mediated activation of the endogenous vasoconstrictor system including RAAS sympathetic nervous system (SNS) and anti-diuretic hormone (ADH) to restore circulatory integrity.
- This causes renal vasoconstriction and renal sodium and water retention.
- This condition will evolve in overt fluid retention and, in the presence of portal hypertension, fluid transudates into the peritoneal cavity with ascites formation.
- Activation of ADH results in a decrease in tubular free water clearance leading to dilutional hyponatremia”, serum sodium level of less than 130 mEq/L).
Pathogenesis of Cirrhotic Ascites
- Ascites may appear suddenly or develop insidiously over the course of months with accompanying flatulent abdominal distension.
- At least 1-2 liters of fluid accumulates in the abdomen before ascites is clinically detected.
- Ascites precedes the development of peripheral edema in cirrhosis.
- Increased abdominal girth.
- Abdominal distention (D.D. obesity, gas, tumors, and pregnancy).
- Full flanks & Scrotal edema.
- Umbilicus becomes everted or bulging.
- Complicated ascites: Complicated ascites is defined as ascites associated with refractoriness to diuretic treatment: Refractory ascites, Hyponatremia, Hepatorenal syndrome, and Spontaneous bacterial peritonitis.
Grades of ascites:
- Grade 1 (mineral ascites): detectable by ultrasound Or Knee-elbow position test.
- Grade 2 (moderate ascites): shifting dullness test.
- Grade 3 (severe ascites): transmitted thrill test.
Hepatic hydrothorax
- Right-sided transudative effusion due to ascitic fluid translocating through diaphragmatic defects from the peritoneum to the pleural space.
- 5-10% of patients with cirrhosis.
- Pulmonary complaints (e.g. dyspnea).
- High serum-pleural albumin gradient ≥ 1.1 g/dl).
- Spontaneous bacterial empyema may be a complication.
- Therapy corresponds to that of ascites.
Diagnosis
Clinical examination
a) History:
- Increase in abdominal girth.
- Diuretic therapy
- Paracentesis.
b) Physical examination:
- Tests for ascites.
- Ascites grades.
Radiological examination
a) Abdominal sonography
- First-line investigation.
- Demonstrates as little as 100 mL of ascites.
- With massive ascites, floating intestinal loops are found.
b) CT scan
- Detects as little as 25 mL of ascites.
- Only indicated in problems with the differential diagnosis (e.g., in acute pancreatitis or suspected tumors).
Ascitic fluid analysis
(A diagnostic paracentesis at the time of first presentation of grades 2 and 3 as well as evaluating for possible complications such as SBP or renal failure).
a) Biochemical analysis
- Microscopic appearance (clear, pale yellow, opaque, bloody or chylous).
- Cell count with differential (PMN in SBP, lymphocytes in TB).
- Albumin, total protein.
- Lactate dehydrogenase) (LDH) (increased in malignant ascites).
- SAAG = Serum Albumin Gradient: In cirrhotic patients with mixed ascites (2 causes or more), SAAG is high. (SAAG Cut- off gradient 1.1g/dl).
- Ascites is classified into: A High SAAG (> 1.1g/dl) = Portal hypertensive ascites, and Low SAAG (<1.1g/dl) = non-portal hypertensive ascites
Special tests
- Glucose (decrease in Infection, TB, malignancy).
- PCR for TB & Amylase for pancreatic disease.
- Triglycerides and cholesterol levels (chylous and pseudochylous ascites).
- Alpha-fetoprotein (HCC).
- Carcinoembryonic antigen (metastasis).
- Hyaluronic acid (mesothelioma).
b) Cytologic analysis
The normal epithelial cells in the peritoneum can resemble malignant cells, so leading to an over-diagnosis of cancer.
c) Bacteriologic analysis
Cultures (10-20 mL of ascitic fluid should be inoculated into two [aerobic and anaerobic] blood culture bottles at the bedside).
Prognosis of cirrhotic ascites
- Ascites is associated with a mortality rate of 50% and 80% within 2 and 5 years respectively after the first ascites episode.
- Persistent ascites and low serum sodium (<126 mEq/L), SBP and renal impairment identify patients with cirrhosis with high mortality risk.
Treatment of ascites in cirrhosis
- The aim is to create a negative sodium and water balance.
- Before discussing the specific treatment of ascites in patients with cirrhosis, it is mandatory to treat underlying cause of liver disease.
- Grade 1 ascites: no treatment.
- Grade 2 ascites: sodium restriction and diuretic therapy.
- Grade 3 ascites: large-volume paracentesis followed by sodium restriction and diuretic therapy.
1. General measures
- Rule out SBP & exclude associated causes of ascites.
- Maintain a protein intake of (1.2-1.5 g/kg, as ascites is a surrogate for protein-deficient malnourishment and always in the setting of hypoalbuminemia.
- Cessation of alcohol use.
- Monitor renal function and electrolytes.
- Discontinue NSAID, ACE inhibitors, and angiotensin receptor blockers.
- Discontinue ẞ-blockers only in the presence of low MAP (mean arterial pressure), infection and acute kidney injury.
Bed Rest
Upright posture activates sodium-retaining systems and impairs renal perfusion and sodium excretion.
3. Sodium restriction (negative sodium balance)
- Daily sodium intake of 80-120 mmol (4.6-6.9 grams of salt/day.
- No added salt in the diet and avoidance of preprepared foodstuffs, A greater reduction in sodium intake is not advisable as it interferes with nutrition.
- In the presence of dilutional hyponatremia (120-125 mmol/L) fluid should be restricted to 1000 ml/day.
4. Diuretic Therapy
- Aldosterone antagonists, such as spironolactone, are used for first-line diuretics to treat.
- Serum electrolytes and renal function should be monitored to prevent over-diuresis, electrolyte disturbances and possible pre-renal azotemia (high level of nitrogen waste products in the blood).
- Monotherapy with furosemide is less effective than the use of spironolactone and is not recommended.
Proper diuretic response
- Daily weight loss of 500 g/d in patients without peripheral edema and 1 kg/d in those with peripheral edema.
- Urinary excretion of sodium >78 mmol/d.
- Random spot urine sodium/ potassium ratio > 1.
Methods of diuretic therapy
A. Sequential or ‘Stepped care’ approach (Grade 2 ascites):
- Spironolactone 100 mg/day as initial dose, if No response for 7 days, 200 mg/day.
- Gradually increasing with/100 mg/week until adequate natriuresis is achieved (max dose 400 mg/d).
- Insufficient response in the first 2 weeks, add furosemide 40mg/d with increasing every 2-3 days (max: 160 mg/d).
B. Combined treatment approach (Grade 3 or recurrent)
- Spironolactone 100 mg/d and furosemide 40 mg/d.
- Dose titration can be performed after 5-7 days with increasing doses to the maximum doses.
5. Large volume paracentesis (LVP) (Grade 3 ascites)
- LVP is for grade 3 ascites followed by sodium restriction and diuretic therapy.
- Total volume paracentesis (complete removal of ascites with only one tap) gives better results in patients with ascites and peripheral edema.
- Albumin infusion is administered If more than 5 liters are drained (8 g/L of ascitic fluid removed) to prevent post-paracentesis circulatory dysfunction due to a rapid decrease of effective arterial blood volume.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Cardio-Pulmonary problems in Liver Cirrhosis and Hepatopulmonary syndrome
Gastro-esophageal varices cause, treatment, and therapy of variceal bleeding
Liver Cirrhosis causes, symptoms, treatment & stages, Liver Biopsy and treatment of PHTN
Viral hepatitis, HDV symptoms, Treatment of acute HCV, Occult hepatitis C and HEV
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Liver development, congenital anomalies, function & Pancreas development