Septic Arthritis definition, symptoms, stages, types and treatment
Septic arthritis can come from germs that travel through your bloodstream from another part of your body, It is a painful infection in a joint, It can occur when a penetrating injury, such as an animal bite or trauma, delivers germs directly into the joint, Infants and older adults are most likely to develop septic arthritis.
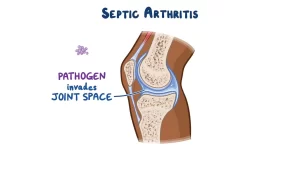
Septic Arthritis
Septic Arthritis is inflammation of a synovial membrane with purulent effusion into the joint capsule, due to infection (A joint inflammation due to an infection usually involving synovial joints).
Anaerobic and gram-negative infections are common in immuno-compromised persons. Although Gonococcal infection is the most common, it has less morbidity and mortality Inflammation of a single large joint (Especially the knee) may be present in Lyme disease.
Involved joints
The most common joints involved in:
- Adults: knee (53%), Hip (20%), Elbow (17%) and Shoulder (10%).
- Children: Knee (39%) and Hip (32%).
Epidemiology and risk factors
1. Common age groups
- 50% of cases: Children less than 5 years.
- 30% of cases: Children less than 2 years.
2. Risk factors for joint infections
i) Factors related to the joint
- Previous arthritis.
- Trauma.
- Prosthetic joint.
ii) Factors related to the patient’s general condition
- Diabetes Mellitus.
- Immuno-suppression.
- Bacteremia.
- Sickle cell anaemia.
Pathogenesis:
1. Mode of the spread of infection to the affected joint:
- Direct invasion.
- Local spread from adjacent tissues.
- Spread from metaphyseal osteomyelitis.
- Hematogenous spread.
- Penetrating damage by puncture or cutting.
- During diagnostic or therapeutic measures.
2. Steps of acute Suppurative arthritis
- Early stage, there is acute synovitis with a purulent joint effusion.
- Soon the articular cartilage is attacked by bacterial and cellular enzymes.
- If infection is not arrested, the cartilage may be completely destroyed.
- Healing then leads to ankylosis.
Patients with rheumatoid arthritis especially those on corticosteroids may develop Silent joint infection.
Complications
- Cartilage destruction may lead to either fibrosis or bony ankylosis.
- In adults, partial destruction of the joint will result in/secondary osteoarthritis.
- Bone destruction and dislocation of the joint (Especially Hip).
- Growth disturbance presents as: either localized deformity or shortening of the bone.
- If left untreated, it will spread to the underlying bone and out of the joint to form an abscess and sinus.
Healing:
Healing occurs with:
- Complete resolution.
- Partial loss of articular cartilage and fibrosis of joint.
- Loss of articular cartilage and bony ankylosis.
- Bony destruction and permanent deformity.
Investigations
1. Lab investigations
i) Blood analysis
- Leucocytosis > 12.000/mm³
- ESR > 40 mm/hr.
- CRP is elevated.
- A blood culture may be positive.
ii) Synovial fluid analysis
- The aseptic technique is used during aspiration of synovial fluid.
- Avoid taking from the infected site of the skin.
- The fluid is then analyzed by:
- Gross examinations: appearance, volume, Viscosity, mucin clotting (amount of proteoglycans).
- Microscopic examination: leucocyte count, Staining of smears.
- Biochemical examination: serum, glucose ratio, protein.
- Culture and sensitivity for definitive diagnosis and treatment.
2. Imaging
i) Plain X-ray:
Early Stage: Normal, Look for:
- soft tissue swelling.
- loss of tissue planes.
- widening of joint space and
- Slight subluxation due to fluid in the joint.
- Gas may be seen with E. coli infection.
Late stage (After 2-3 weeks):
- Joint space narrowing.
- The blurring of fat planes.
- Increased density of fatty marrow.
- Periosteal reaction.
- Cortical erosion or destruction.
ii) Ultrasound
Value:
- Ultrasound should be the first line of investigation in a suspected case of infective arthritis as it is economical, available, accurate, and safe
- It is more reliable in revealing a joint effusion in early cases.
Findings:
- It can detect joint swelling.
- Widening of space between the capsule and bone > 2 mm indicates effusion.
- Echo-free indicates transient synovitis.
- Positively echogenic indicates septic arthritis.
iii) Computed tomography (CT)
Value:
CT is used to: guide joint aspiration, monitor therapy, and plan operative approaches.
Findings:
- Soft tissue swelling.
- Joint effusions.
- Abscess formation.
iv) MRI
Value:
- MRI shows extent of infection.
- It diagnoses infections that are difficult to access.
- It shows better anatomical details).
Findings:
- Synovial enhancement.
- Peri-synovial edema and joint effusion.
- Single or multiple radiolucent abscesses.
Nuclear medicine imaging
Value:
- Nuclear medicine imaging can detect septic arthritis: 10-14 days before changes are visible on plain radiographs.
- Highly sensitive but non-specific.
- Inexpensive
Findings:
- Focal hyperperfusion.
- Focal hyperemia.
- Focal bone uptake.
Differential diagnosis
Septic arthritis must be differentiated from Reactive arthritis, acute osteomyelitis, trauma, irritable joint, hemophilic joint, rheumatic fever, gout and pseudo-gout, and Gaucher’s disease.
Treatment
If the history and diagnostic studies suggest an infection, aggressive treatment can prevent rapid joint destruction.
- General supportive measures: Analgesics, and IV fluids.
- Splintage: The joint must be rested either on a splint or in a widely splint plaster. In neonates and infants with hip infection, the joint is held abducted and 30 degrees flexed on traction to prevent dislocation.
- Antibiotics: Treatment is started once the blood and samples are obtained without waiting for the detailed results, The choice of antibiotics depends on the most likely pathogen.
- Surgical management:
- Surgical Drainage: Indications: Joints that don’t respond to antimicrobial therapy and daily arthrocentesis, Any joint with limited accessibility, including the sternoclavicular or the hip joint. Patients with underlying diseases (DM, RA, Immuno-suppression) need more aggressive treatment with earlier surgical intervention.
- Arthroscopic debridement and copious irrigation with normal saline, more frequently in the knee joint septic arthritis.
Gonococcal arthritis
It is the most common type of septic arthritis in the young, it is three to four times more common in women than in men.
- Causative organism: It results from gonococcal infection (Colonization of the urethra, cervix, and pharynx).
- Causes: Common in: Sexually active healthy persons, Congenital complement component deficiency.
- Clinical features: Disseminated gonococcal infection: Acute illness with: fever, chills, and malaise. Tenosynovitis of the knees, hand, wrists, feet and ankles, Generalized Arthralgia polyarthralgia syndrome, Migratory arthritis, Dermatitis (Pustular or Vesiculopustular), a small number of papules that progresses to haemorrhagic pustules present on trunk and extensor surfaces of distal extremities).
- Treatment: Initially, Ceftriaxone (1 g IV every 24 h). When local and systemic signs resolve → oral antibiotic (Ciprofloxacin 500 mg BD) should be started for 7 days. In Penicillin susceptible: Amoxacillin 500 mg TDS. Suppurative arthritis usually responds to needle aspiration and antibiotic treatment for 7-10 days.
Mycobacterial arthritis
It represents 1% of all cases of TB and 10% of extra-pulmonary cases.
1. Causative organism: It enters the body via the lung (Droplet infection) or the gut (Swallowing infected milk products), rarely through the skin.
2. pathology: TB causes granulomatous infection associated with tissue necrosis and caseation.
- Iry complex: Initial lesion in lungs, pharynx, or gut with lymphatic spread to regional LNs.
- 2ry spread: Widespread dissemination via blood stream giving rise to extrapulmonary lesions.
- Tertiary lesion: Foci developing into destructive lesions. Once they get a foothold → they elicit a Chronic inflammation.
Pathology of joint
When the synovium is involved, it becomes thick and edematous with marked effusion, then the pannus of granulation tissue develops, articular cartilage is slowly destroyed, and increased vascularity causes osteopenia.
if unchecked, caseation and infection extend into surrounding soft tissues to produce a cold abscess that may burst forming a sinus and tuberculous ulcer.
3. Clinical features:
- Previous infection or recent contact with TB.
- A long history of pain and swelling.
- Marked synovial thickening.
- Involvement of only one joint.
- Severe muscle wasting
- Enlarged and matted regional LNs.
- Night cries, fever, night sweats, loss of weight.
4. Investigations:
X-ray:
- Soft tissue swelling.
- Periarticular osteoporosis,
- articular space narrowing.
- epiphyseal enlargement in children,
- Erosion of subarticular bone.
- Little or no periosteal reaction.
5. Treatment:
- Rest.
- Chemotherapy: 2 months course of Isoniazid, Pyrazinamide, and Ethambutol 3 times weekly, and then 4 months course of Isoniazid, ethambutol, and Rifampicin.
Fungal arthritis
1. Causative organism
Superficial Mycoses: Primarily infection of the skin and mucous membrane (Candida, Actinomycoses).
Deep Mycoses: (Blastomyces, Histoplasma, Cryptococcous, Aspergillus, Coccidioides) →They gain entry through the lungs.
2. Pathology
The infection causes granulomatous reactions, often leading to abscess formation, tissue destruction, and ulcer formation.
3. Pathogenesis
Cut in foot → spread infection through subcutaneous tissues and along tendon sheaths.
Bones and joints are infected by direct invasion.
local abscesses form and break through the skin as multiple sinuses
4. Clinical features
Subcutaneous nodule: which is tender with a swollen foot, indurated, with discharging sinuses and ulcers.
5. Investigations
- X-ray: Multiple bone cavities and progressive bone destruction.
- Organisms can be identified in sinus discharge or biopsy.
6. Treatment
- IV Amphotericin.
- Necrotic tissue is excised.
- Amputation may be necessary.
A 56-year-old man with fungal arthritis of the right knee due to Candida infection.
- X-ray showed degenerative arthritis of the bilateral knee.
- Representative isolates of Candida were cultured from the fluid in the Sabouraud medium.
Candidiasis
1. Causative organism
- Normal commensal organisms.
- Gain entry through direct contamination during surgery or other invasive procedures.
- Immunosuppression is a predisposing factor.
2. Diagnosis
Tissue sampling and culture.
3. Treatment
- IV Amphotericin B.
- Joint irrigation.
- Curettage.
Viral arthritis
Infects synovial tissue during systemic infections or by provoking an immunologic reaction that involves joints.
1. Causative organism
Rubella: Arthralgia, frank arthritis within 3 days of rash following natural infection with rubella.
Parvovirus B-19: Arthritis, arthropathy, stiffness of joints.
Acute Hepatitis B: Arthralgia, fever, urticaria 2 weeks before onset of jaundice.
Hepatitis B: Sudden symmetrical polyarthritis of the small joints of hands in one-third of patients.
HIV Infection: Infective arthritis, minimal or no symptoms, Some recent anti-viral agents cause arthritis (Crystallization in joints). Arthralgia is common in AIDS (usually seronegative) in Lower Limbs similar to Reiters or Reactive arthritis.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Magnetic Resonance Imaging (MRI) uses, advantages and disadvantages
Computed Tomography (CT scan) types, uses, advantages and disadvantages
Cone beam CT vs. Fan beam CT, CBCT advantages, disadvantages, and uses
What is PET/CT, Positron emission tomography scan (PET) uses, risks, and importance