Pancreatic secretion composition, regulation, function, Differences between jejunum and ileum
The exocrine pancreatic secretion is considered the most important source of the digestive enzymes of the gastrointestinal tract. It is poured into the lumen of the small intestine. Pancreatic secretion contains enzymes for digesting the three major types of food: proteins, carbohydrates, and fats. It contains large quantities of bicarbonate ions, which have an important role in neutralizing the gastric acid chyme in the duodenum.
Exocrine pancreatic secretion
The exocrine portion of the pancreas consists of alveolar glands (acini) containing digestive enzymes in the form of (zymogen granules) which are discharged from the cells into the lumen of the pancreatic ducts. The small ducts unite together forming a single duct, the main pancreatic duct, which usually joins the common bile duct to form the ampulla of Vater.
The ampulla opens through the duodenal papilla, this opening is encircled by the “sphincter of Oddi”. Sometimes there is an accessory pancreatic duct that opens in the duodenum more proximally.
Composition of pancreatic secretion
Pancreatic secretion is the most alkaline juice in the human body, About 1500 ml of pancreatic juice is secreted daily. Its pH is 8.3, It contains sodium bicarbonate in a concentration about 5-fold that of plasma, The flow of gastric acid chyme into the duodenum is the main stimulus for bicarbonate secretion.
Bile and intestinal juices are also neutral or alkaline, and these three secretions neutralize the gastric acid, raising the pH of the duodenal contents to 6.0 to 7.0, The main enzymes present in pancreatic secretion are:
1. Proteolytic enzymes
Trypsinogen
It is secreted in an inactive form and then activated to trypsin by an enzyme present in the intestinal secretion called enterokinase. Any amount of trypsin formed auto-activates the rest of the trypsinogen present, and also activates other proteolytic enzymes. The optimum pH for its action is between 8 and 9. It converts proteins into peptides of various sizes, but does not cause the release of individual amino acids. It is an endopeptidase.
Chymotrypsinogen
It is secreted in an inactive form, and activated into chymotrypsin by trypsin. It is also an endopeptidase. It acts specifically on peptide linkages, which contain aromatic amino acids. Each proteolytic enzyme completes the action of the other.
Pro carboxypeptidase
This enzyme is activated by trypsin into carbyxypolypeptidase. It is an exopeptidase because it hydrolyses polypeptides separating the amino acid with a free carboxylic group.
Proelastase
This enzyme is activated by trypsin to the active form of elastase. It attacks the elastic fibers. It cleaves peptide bonds of aliphatic amino acids.
e. Ribonucleases and deoxyribonucleases
Nucleases split the two types of nucleic acid, ribonucleic and deoxyribonucleic acids into nucleotides.
2. Pancreatic amylase
This enzyme hydrolyses starches, glycogen, and most other carbohydrates except cellulose to form oligosaccharides (maltose, maltotriose and a-dextrins). Chloride ions serve as a coenzyme for it. It has a more powerful action than salivary amylase; it can split the uncooked starch.
3. Lipolytic enzymes
- Pancreatic lipase: This enzyme hydrolyzes triglycerides (triacylglycerols) to free fatty acids and 2 monoglycerides (2-monoacylglycerols). Colipase is also secreted in the pancreatic juice, and when it binds to pancreatic lipase, it facilitates its action.
- Cholesterol esterase: Catalyzes hydrolysis of cholesterol esters.
- Phospholipase: Splits fatty acids from phospholipids.
Other constituents of pancreatic juice
- Water.
- Cations as Na+, K+, Ca++, Mg++.
- Anions such as HCO3−, CI−, SO4−, and HPO4−.
- Albumin and globulin.
Secretion of trypsin inhibitor
Once trypsin is activated, there is an autocatalytic chain reaction. The release of any minute amount of trypsin into the pancreas is very dangerous because it gives many active enzymes which might digest the pancreas itself. However, activation of proteolytic enzymes occurs only in the intestine.
This is because the pancreatic acini that secrete the enzymes secrete at the same time a trypsin inhibitor, this substance is stored in the cytoplasm of the glandular cells surrounding the zymogen granules, and prevents activation of trypsinogen in the pancreas, thus protecting it from autodigestion.
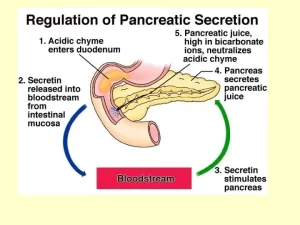
Regulation of pancreatic secretion
Pancreatic secretion, like gastric secretion, is regulated by both nervous and hormonal mechanisms, but hormonal regulation is more important. Little secretion elaborates during fasting. After intake of the meal, pancreatic secretion starts after a few minutes by reflex action. Then the flow of juice is augmented when the acid chyme enters the duodenum. The secretion reaches a maximum level 3 hours after meals and greatly declines when the stomach is emptied.
1. Nervous regulation
The nervous type of secretion occurs by both conditioned and unconditioned reflexes, it is abolished by atropine, The same nervous signals from the brain that cause secretion in the stomach also cause acetylcholine release by the vagal nerve endings in the pancreas, It stimulates pancreatic acinar cells to cause the discharge of zymogen granules, The nervous type of secretion is small in amount, rich in enzymes but deficient in alkali and water.
2. Hormonal regulation
Evacuation of the gastric contents to the duodenum leads to copious pancreatic secretion. Some local hormones evoke pancreatic secretion (mainly secretin, CCK, and VIP). It could be divided into the gastric phase via gastrin which increases pancreatic juice rich in enzymes, and the intestinal phase via secretin, CCK, and VIP.
A. Secretin
It is a polypeptide of 27 amino acids, Secretin is secreted by S cells that are located in the mucosa of the upper portion of the small intestine, It is present in an inactive form, pro-secretin, The entry of acid chyme to the duodenum leads to the release and activation of secretin, It circulates in the blood and reaches the pancreas via its arterial blood supply.
Actions of secretin
Pancreatic actions of secretin
Secretin causes copious secretion of a very alkaline pancreatic juice poor in enzymes, It is believed to act on duct cells which probably secrete water and bicarbonate, The release of secretin by acid is an example of negative feedback control, Secretin causes alkaline pancreatic juice to flood into the duodenum neutralizing the acid from the stomach and thus inhibiting further secretion of the hormone.
What is the importance of this large volume of alkaline pancreatic secretion?
- It neutralizes the acidity and blocks peptic gastric activity since the intestinal mucosa can’t withstand the digestive properties of the acidic gastric juice. This acts as a protective mechanism against duodenal ulceration.
- Bicarbonate secretion by the pancreas after secretin provides the suitable pH for the action of the pancreatic enzymes which act optimally at a pH of about 8.
- It augments CCK actions on the pancreas.
Extra-pancreatic action of secretin
- It stimulates bile secretion: mainly its water and bicarbonate content, but the output of bile salts, and bile pigments does not increase i.e. hydrocholeretic action.
- It decreases intestinal movements.
- It decreases gastric acid secretion and may cause contraction of the pyloric sphincter.
B. Cholecystokinin (CCK)
Cholecystokinin hormone is released from the I cells at the mucosa of the upper small intestine in the presence of digestive products or proteins, and fats, In addition to its secretion by I cells in the upper intestine, CCK is found in nerves in the distal ileum and colon, It is also found in neurons in the brain, especially the cerebral cortex, and in nerves in many parts of the body.
Actions of CCK
Pancreatic actions of CCK: Cholecystokinin evokes pancreatic secretion rich in enzymes and poor in water and bicarbonates, which is similar to the effect of vagal stimulation, Because the bile and pancreatic juice that enter the duodenum in response to CCK further catalyze the digestion of more protein and fat.
The products of this digestion stimulate further CCK secretion, a sort of positive feedback that operates in the control of the secretion of this hormone, However, the positive feedback is terminated when the products of digestion move on to the lower portions of the gastrointestinal tract, It also augments the action of secretin on the pancreas, In addition, CCK stimulates the release of glucagon.
Extra-pancreatic actions of CCK
- Helps evacuation of the gall bladder, i.e. cholagogue.
- Increases intestinal movements.
- It inhibits gastric motility, emptying, and secretion, It augments the contraction of the pyloric sphincter, thus preventing the reflux of duodenal contents into the stomach.
- It may be involved in the regulation of food intake, and it appears to be related to the production of anxiety and analgesia.
C. Vasoactive intestinal peptide (VIP)
It stimulates the secretion of water and bicarbonate from the pancreas, but it is weaker than secretin. VIP is found in certain neurons and endocrine cells throughout the intestine.
II. Mobile part of the small intestine
Jejunum and ileum
They form the mobile part of the small intestine, suspended from the posterior abdominal wall by a mesentery.
Differences between jejunum and ileum:
Jejunum:
- Length: The proximal 2/5.
- Diameter: thick wall and wide lumen.
- Arterial arcades: Few and simple.
- Mesentery: Few fat, presents windows.
- Mucosal Circular Folds: Numerous.
- Peyers Patches submucosal aggregations of lymphoid tissue: No.
ileum:
- Length: The distal 3/5.
- Diameter: thin wall and narrow lumen.
- Arterial arcades: Numerous and complex.
- Mesentery: Much fat, no windows.
- Mucosal Circular Folds: Few.
- Peyers Patches submucosal aggregations of lymphoid tissue: Numerous Peyer’s patches.
Mesentery of the small intestine
It is a fan-shaped peritoneal fold that has an anterior free border and a posterior attached border. The anterior border contains coils of jejunum and ileum and is 6 meters long. The posterior border is attached to the posterior abdominal wall..the root of the mesentery and is about 6 inches long.
Borders:
1. Attached border (called the root of mesentery): It is 6 inches, and extends from the duodenojejunal flexure to the iliocaecal junction.
Structures crossed by the root of the mesentery (6):
- 3rd part of the duodenum.
- Abdominal aorta and right gonadal vessels.
- IVC.
- Right psoas major.
- Right ureter.
- Right genito-femoral nerve.
Contents of the mesentery
- Superior mesenteric artery.
- Superior mesenteric vein.
- Coils of the small intestine.
- Extraperitoneal tissue and fat.
- Sympathetic nerve fibers.
- Mesenteric LN (arranged in three groups: large, medium, and small).
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Bile salts & gall bladder function, Factors affecting gall bladder evacuation (Cholagouges)
Histological structure of gallbladder and Pancreas, Functions of the liver & Composition of bile
Histology of pancreas, Structure of islets of Langerhans, Insulin function & Metabolism
Pancreas function, anatomy, parts, relations, ducts & blood supply