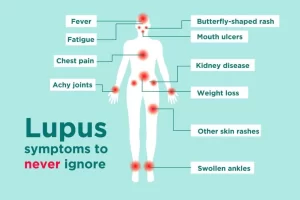
Systemic lupus international collaborating clinics classification, Lupus and antiphospholipid syndrome
Systemic Lupus International Collaborating Clinics (SLICC) encompasses 11 Clinical and 6 Immunological criteria, The patient should satisfy at least FOUR of the criteria including one clinical criterion and one immunological criterion, Biopsy proven Nephritis compatible with SLE in the presence of ANA or Anti-dsDNA antibodies in the absence of other lupus features is regarded as sufficient for a patient to be diagnosed as having lupus.
SLICC’ Classification Criteria for Systemic Lupus Erythematosus
Requirements: ≥ 4 criteria (at least 1 clinical and 1 laboratory criteria) OR biopsy-proven lupus nephritis with positive ANA or Anti-DNA.
Clinical Criteria
- Acute Cutaneous Lupus.
- Chronic Cutaneous Lupus.
- Oral or nasal ulcers.
- Non-scarring alopecia.
- Arthritis.
- Serositis.
- Renal.
- Neurologic.
- Hemolytic anemia.
- Leukopenia.
- Thrombocytopenia. (<100,000/mm³).
Immunologic Criteria
- ANA.
- Anti-DNA.
- Anti-Sm.
- Antiphospholipid Ab.
- Low complement (C3, C4, CH50).
- Direct Coombs’ test (do not count in the presence of hemolytic anemia).
Treatment
Therapeutic principles (Important concepts)
Goals of therapy:
- Stop and reverse ongoing organ inflammation.
- Prevent or limit irreversible end-organ damage.
Potential toxicities of immunosuppressive therapies demand vigilant management.
Strategic use of targeted immunobiological therapies based on pathogenic mechanisms vs global Immunosuppression.
Management
There is NO cure. Complete sustained remission is RARE. Mainstay: Suppression of symptoms and Preventing organ damage. It depends on the severity of the disease. It aims at preventing complications of diseases and their treatment.
Non-life (OR organ) threatening: Non-pharmacological conservatives and Risk factor modification→Addition of low-dose Corticosteroids or Belimumab.
Life (OR organ) threatening: Nephritis, Myelitis or Vasculitis. High-dose IV steroids and aggressive immunosuppressant.
Special conditions: Pregnancy, Dermatitis or Thrombotic crisis.
Non-pharmacological management
- Sunscreens or Sun protection factors (SPF): At least 30, the Preferred more than 55.
- Smoking cessation.
- Weight loss.
- Exercise.
- Optimal blood pressure (BP) control.
- Supplemental Vitamin D.
- Avoid: high-dose oestrogen therapy or oral contraceptives.
- Avoid Culprit meds: Sulphonamides.
- Avoid pregnancy.
The Recommendations (T2T)
- Prevention of disease flares, and particularly severe flares of nephritis, neuropsychiatric symptoms, and SLE overall.
- Some interventions can prevent at least some flares with a reasonable balance of risks/side effects.
- Prevention of damage was also addressed and accorded considerable importance because of the associations between organ damage and poor prognosis.
- Patients who are e clinically asymptomatic should be monitored closely but are at risk for overtreatment if serology alone guides treatment.
- Promptly evaluate the renal function for all patients because of evidence in the literature suggesting that each 1-month delay in diagnosis and initiating immunosuppression increases the risk of relapse (RR1.03).
- Lupus nephritis consists of both induction and maintenance, and, in general, the maintenance phase should include at least 3yrs of treatment.
- Using the lowest dose of steroids that can control the disease and recommended that most patients be on anti-malaria if not contraindicated.
- Treatment of comorbidities, such as antihypertensives and lipid-lowering agents.
Guiding Therapeutic Strategies
- Therapeutic combinations aimed at induction of remission, maintenance therapy, and supportive therapy.
- Titrate dose to treat effectively with a focus on involved organs, and to minimize toxicity.
- Strategic use of preventive therapies, antibiotics, and vaccinations.
- Cardiovascular screening.
- Cancer screening.
- Osteoporosis screening.
Pregnancy and Lupus
Lupus does not affect fertility. The rate of fetal loss Increased. Demise is higher in mothers with High disease activity, SLE nephritis, and APLA (Antiphospholipid syndrome). Women with Anti-Ro SSA need additional monitoring, a high risk for neonatal Lopus. APLA with SLE treated with heparin and low-dose Aspirin.
- Fertility is not affected.
- Increased incidence of abortion prematurity.
- SLE flare may occur during pregnancy. DD lupus flare from pre-eclampsia.
In flare:
- Other signs of activity of SLE.
- Low complement.
- Raised anti-dsDNA titer.
Disease activity should be controlled before conception. Anticardiolipin and lupus anticoagulants should be investigated. If positive give low dose aspirin ± low molecular weight heparin are used.
Neonatal Lupus
- Trans-placental fluorinated corticosteroids, dexamethasone, and betamethasone.
- Hydroxychloroquine during pregnancy is associated with reduced rates of NLS.
- IVIg was reported to prevent recurrence of CHB (complete heart block) in one study, but two large RCTs Failed to show any beneficial effect.
Monitor fetal heart sounds: fetal heart block may occur as a manifestation of neonatal lupus.
Drug-Induced Lupus
- Appears during therapy.
- Fever, malaise, arthritis, intense arthralgia, myalgia, serositis, and or rash (less common).
- ANA’s positivity is very high.
- Differs from SLE, White predominance, less female predilection, rare involvement of kidneys or brain. Commonly Antihistone antibody positive. Anti-dsDNA and RNP are rare.
Management
- Withdraw the offending drug.
- Low doses of systemic corticosteroids if severe disease.
- Drugs: Hydralazine-Procainamide -Isoniazid-Hydantoin -Chlorpromazine- α Methyldopa-D penicillamine-α interferon.
- Clinical and serological manifestations of SLE improve quickly upon discontinuing the drug.
- Clinical: constitutional symptoms, fever, arthritis, serositis but no renal or CNS manifestations and Equal male to female ratio.
- Serological:
- (+) ve ANA, anti-ssDNA, anti histone.
- (−) ve anti ds DNA.
- No reduced complement.
Microvascular Thrombotic Crisis
- Hemolysis, thrombocytopenia, and microvascular thrombosis in kidneys, brain, and other tissues.
- High mortality.
- LAB: Peripheral smear shows schistocytes, LDH is elevated, Antibodies to ADAMTS13.
- Management: Plasma exchange along with GC therapy.
Lupus and antiphospholipid syndrome
- Repeated fetal losses, venous or arterial clotting, with at least 2 positive tests for APLA (12 weeks apart).
- Target INR: Between 2.0 – 2.5 (One episode of venous clotting). Between 3.0 – 3.5 (recurring clots or arterial clotting).
- Heparin and Warfarin.
- Statins, hydroxychloroquine, and rituximab might be useful.
Antiphospholipid syndrome
- Recurrent arterial or venous thrombosis.
- Recurrent abortions.
- Thrombocytopenia.
- Presence of anticardiolipin (IgG, IgM) antibodies or lupus anticoagulant.
Antibodies against cell surface antigens
- RBCS → Coomb’s positive hemolytic anemia.
- Platelets → thrombocytopenia.
- Lymphocytes → lymphopenia.
- Neuronal cells → antineuronal antibodies with diffuse CNS disease.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Systemic Lupus Erythematosus symptoms, diagnosis, types and treatment
Rheumatoid Arthritis (RA) causes, stages, symptoms, diagnosis, and specific joint affection
Rheumatoid Arthritis diagnosis and treatment, Disease-Modifying antirheumatic drugs (DMARDs)
Non-radiographic axial spondyloarthritis, Reactive arthritis, and Enteropathic arthritis