Upper and lower motor neurons lesion, Stages of complete spinal cord transection
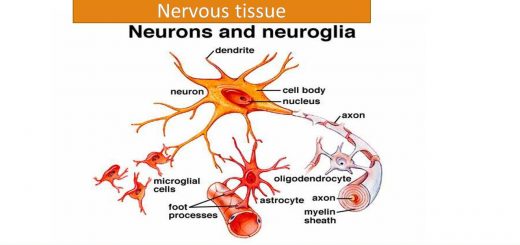
Upper motor neuron refers to the motor neurons of the cerebral cortex and their axons which terminate at the brainstem and spinal cord while the lower motor neuron refers to the motor nuclei of cranial nerves and their axons as well as the anterior horn cells of the spinal cord and their axons.
Upper motor neuron lesion
Upper motor neuron lesion (UMNL) means lesions that affect the cortical motor areas or the pathways of the descending tracts in the brain or spinal cord.
Causes: vascular, trauma, tumor, or degenerative diseases. The most common lesions are lesions of the internal capsule commonly caused by vascular disorders.
Manifestations
- Paralysis: On the opposite side of the lesion (due to crossing of the motor tract). Widespread (pyramidal fibers form a compact bundle that occupies a small area).
- Increased (exaggerated) deep reflexes and may be clonus: due to the state of supraspinal facilitation which increases the activity of muscle spindle to stretch.
- Plantar reflex: extensor plantar responses (positive Babinski sign). Babinski sign is a part of the spinal withdrawal reflex which in the normal subject is inhibited by the corticospinal tract.
- Superficial reflexes: superficial reflexes as abdominal reflexes are lost because superficial reflexes receive facilitatory influence from the pyramidal tract.
- Muscle status: there is no or little wasting.
- Increased tone spasticity:
- Decrease of the extrapyramidal inhibitory discharge (from the inhibitory reticular formation on the gamma efferent while the facilitatory discharge continues (from the facilitatory reticular formation).
- In UMNL there is increase facilitatory discharge to the gamma motor neurons causing Increased sensitivity of muscle spindle. Clasp knife effect could be elicited. Normally the facilitatory reticular formation discharges spontaneously. The inhibitory reticular formation that decreases the gamma efferent discharge does not discharge spontaneously but is driven instead by fibers from the cerebral cortex.
- In UMNL there is an interruption of the cortical discharge to the inhibitory reticular formation which decreases its activity. Hence the balance between inhibition and facilitation shifts towards facilitation and the gamma efferent discharge is increased. Furthermore, the vestibulospinal tracts remain intact and they also have a facilitatory effect on muscle tone.
Lower motor neuron lesion
Lower motor neuron lesion (LMNL) means a lesion or damage to the lower motor neurons in the spinal ventral horn (or motor nerve innervating a given muscle) or the corresponding motor nuclei of cranial nerves in the brainstem.
Causes: poliomyelitis or trauma to peripheral nerves.
Manifestations:
- Paralysis: on the same side and localized (at the level of the lesion).
- Decreased tone (hypotonia) or flaccidity: due to cut of the stretch reflex arc.
- Decreased or (absent) deep reflexes in the affected segment.
- Plantar reflex: either normal or absent if the involved muscles are paralyzed.
- Superficial reflexes: lost in the affected segment (if they involve contraction of the denervated muscle).
- Muscle status: there is marked wasting because the muscle is deprived of its motor supply.
- Signs of muscle denervation could be elicited as fasciculation (muscle twitches visible under the skin due to denervation of motor units) and fibrillation (muscles potentials detected electromyography in denervated muscles).
Spinal cord lesions
I. Complete transection of the spinal cord
Spinal cord injury can occur from many causes, including trauma, tumor, ischemia, and demyelinating diseases. If the lesion is above the level of C3, breathing could be affected. Transection in the lower cervical region results in quadriplegia i.e. paralysis of the four limbs. Transection in the thoracic region results in paraplegia i.e. paralysis of both lower limbs.
It is important to remember that the spinal cord ends at the level of the lower border of the L1. Below this level, the spinal canal is occupied by the lower nerve roots. Therefore, injuries to the spinal canal below this level cause a sensory loss in the region of the body innervated by the lower lumbar and sacral nerve roots as well as a lower motor neuron weakness and decreased tendon reflexes in certain leg muscles.
Stages of complete spinal cord transection
A. Stage of spinal shock
When the transection is complete there is usually a period after the accident when all spinal reflexes below the level of the transection are reduced or completely suppressed. This condition is known as spinal shock. This stage is characterized by:
- Loss of all sensations and all voluntary movements below the level of the lesion.
- Loss of cord reflexes as stretch reflex and flexor withdrawal reflex etc.
- Bladder and bowl control are lost. There is urine retention with overflow and dribbling of urine.
- Loss of erection.
- Drop of the arterial blood pressure if the transection is at the level of first thoracic segment due to block of the sympathetic activity, but slight drop occurs if the lesion is below the second lumber segment.
Complications as urinary tract infection and bedsores may occur during spinal shock. Therefore, adequate management of the paraplegic patient is very important to prevent the occurrence of complications.
The duration of spinal shock is much shorter in animals than in human (in animals it lasts for minutes up to hours or day). The long recovery period for humans reflects the greater influence of descending input on spinal reflex circuits. The cause of spinal shock is due to sudden withdrawal of tonic facilitatory influence from the brain
B. Stage of recovery
During the course of weeks and months following spinal shock, the following occurs:
- Recovery of spinal reflexes as the stretch reflex, they are often exaggerated compared with normal.
- The spinal sympathetic vasoconstrictor centers in the lateral horn below the level of the transection regain their activity and send their impulses to the arterioles and veins, which regain tone.
- Micturition and defecation become automatic as in children with residual urine (due to incomplete evacuation).
- Touch of the patient with a noxious stimulus applied to the skin produces a flexor withdrawal reflex and impulses may irradiate to autonomic centers which leads to provocation of a mass reflex i.e. sweating, pallor, swinging blood pressure, micturition, defecation in addition to wide spreading flexor activity as flexor spasm of both lower extremities and contraction of the anterior abdominal wall. It presumably results from the activation of a great number of neuronal circuits that excite large areas of the cord at once: it is similar to the mechanism of epileptic fits that involve circuits in the brain instead of the cord.
- Several mechanisms may contribute to recovery: denervation hypersensitivity to the mediators released by the remaining spinal excitatory endings, increased number of postsynaptic receptors, and the sprouting of collaterals.
II. Hemisection of the spinal cord
If one side of the cord is transected, it leads to a characteristic pattern known as Brown Sequard syndrome; which is caused commonly by trauma, herniated disk, or spinal cord tumor, the following manifestations could be found:
- On the opposite side (contralateral): the sensation of pain and temperature are lost due to the cut of the lateral spinothalamic tract coming from the Intact side.
- Below the hemisection:
- On the same side (ipsilateral):
- Paralysis of voluntary movements due to interruption of the descending motor pathways (UMNL).
- Loss of dorsal column sensations (vibration sense, tactile discrimination, and light touch). However, the spino-thalamic sensations are preserved.
III. Syringomyelia
Syringomyelia is a developmental abnormality that results in a cavity formation in the spinal cord originating in the central canal and is common in the cervical spinal cord.
The cavity interrupts the crossing spinothalamic fibers leading to bilateral loss of pain, and temperature sensations at the level of affected segments, while the dorsal column sensation of the same segments remains intact, so syringomyelia is an example of dissociated anesthesia.
In late stages, the overgrowing tissue extends towards the ventral spinal horn destroying the anterior horn cells producing muscle weakness and may be muscle atrophy at the level of the affected segment.
Reticular formation, Reticular activating system & Types of EEG waves and Phases of sleep
Diencephalon function, Thalamus, Metathalamus, Hypothalamus, Epithalamus and Subthalamus
Function and Physiology of Thalamus, hypothalamus and Limbic system