Reticular formation, Reticular activating system, Types of EEG waves and Phases of sleep
The reticular formation is an anatomic area in the brainstem made up of various neurons and fibers with discrete and multiple functions. It is associated with the regulation of various sensory-motor, arousal, and autonomic functions. It also contains neurons that secrete neuromodulators.
Functions of the reticular formation
- Modulation of muscle tone, reflexes, and posture: the nuclei of the reticular formation, give rise to the reticulospinal tracts of the spinal cord. These tracts function in the regulation of muscle tone, and posture.
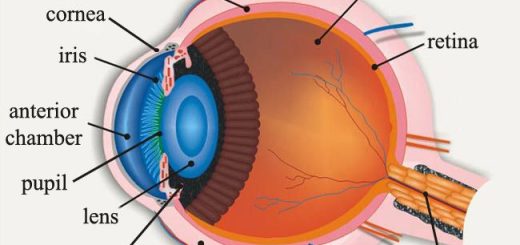
- Control of gaze: nuclei in the pontine reticular formation help in generating conjugate eye movements. They receive input from the superior colliculus and discharge to the ocular motor nuclei.
- Regulation of autonomic functions: the reticular formation includes the cardiac and vasomotor centers, as well as the respiratory centers. It also contains neurons that regulate chewing and swallowing.
- Pain modulation: the reticular formation receives pain and temperature information from the ascending tracts and projects to the intralaminar nuclei of the thalamus, It is also the origin of the descending analgesic pathways where the raphe nuclei and locus ceruleus nuclei contain neurons whose axons synapse onto interneurons in the spinal cord to block the transmission of pain.
- Consciousness: the reticular formation has projections to the thalamus and cerebral cortex through fibers known as the reticular activating system which controls the level of consciousness by regulating arousal and sleep.
Brain areas involved in arousal and sleep
I- Brain areas involved in arousal
The brainstem and hypothalamus promote wakefulness by sending excitatory signals to the cerebral cortex to maintain arousal.
1. The brainstem
a. The reticular activating system:
The brainstem maintains arousal through the reticular activating system (RAS), which is a set of connected nuclei in the upper pons and midbrain. The RAS is composed of several pathways connecting the brainstem to the cortex. These pathways originate in the upper brainstem and project to the intralaminar thalamic nuclei and to the cerebral cortex.
Function of the RAS
The main function of the RAS is to discharge to the thalamus and cortex to stimulate thalamic and cortical activity and promote arousal. Injury to the reticular activating system can result in an irreversible coma. The activity of RAS is affected by several factors:
Factors increasing RAS activity
- Impulses from sensory pathways.
- Impulses from the motor cortex.
- Stress
- Sympathomimetic drugs.
- Caffeine.
- Thyroid hormone.
Factors decreasing RAS activity
- Impulses from medullary and pontine sleep centers.
- Anesthetic drugs.
- Damage to the fibers of the RF in the midbrain or thalamus can lead to coma.
b. Other arousal areas and neurotransmitters in the brainstem:
- Cholinergic neurons in the pontine reticular formation secrete acetylcholine which promotes cortical activation during wakefulness.
- The locus ceruleus which secretes noradrenaline which promotes wakefulness.
- Raphe nuclei which secrete serotonin which promotes wakefulness.
2. The hypothalamus
- Posterior hypothalamus: histaminergic neurons in the posterior hypothalamus maintain wakefulness (This is why antihistaminic drugs induce sleep).
- The lateral hypothalamus: the neurons in the lateral hypothalamus stimulate other wakefulness areas in the brain by releasing the neuropeptide orexin. Orexin promotes wakefulness and its deficiency causes narcolepsy (A condition characterized by a tendency to fall asleep).
Il- Brain areas and neurotransmitters involved in sleep
Certain areas in the brain promote sleep, these areas include:
- The anterior hypothalamus: The preoptic nucleus in the anterior hypothalamus contains neurons that are particularly active during sleep and release the inhibitory neurotransmitters GABA, and galanin to inhibit neurotransmitters of arousal.
- The pineal gland: melatonin is secreted from the pineal gland at night and it is a sleep-promoting factor.
- ADP accumulation in the brain: during prolonged wakefulness, energy-producing brain systems run down and ATP levels are depleted. ADP levels accumulate and extracellular adenosine levels rise with time and it induces sleep (Caffeine blocks adenosine receptors).
- Interleukin-1: it is one of the cytokines which has a role in the body immune system, and was found to promote sleep. CSF levels of interleukin-1 increase during infection, possibly explaining why we sleep more when we are sick.
EEG and sleep
The electrical activity of the brain: The electroencephalogram (EEG) is a recording of the electric activity of the brain. The EEG is recorded using electrodes placed over the scalp at regular distances.
Types of normal EEG waves
There are four types :
- Alpha waves are rhythmic waves occurring at a frequency of 8-13/sec with an amplitude of about 50uV most marked in the parieto-occipital region, Alpha waves are recorded in an awake but mentally and physically relaxed person with eyes closed.
- Beta waves are seen in the frontal regions. They have a frequency of more than 14/ sec and have amplitude lower than the alpha waves. They occur during the activation of the brain.
- Theta waves have frequencies between 4 & 7 cycles per second, They occur normally in children, Theta waves are also seen in many brain disorders.
- Delta waves have frequencies of about 1-3/sec, with high amplitude. They occur in very deep sleep in adults, in infancy, and in brain diseases.
Based on EEG changes there are 2 distinct phases of sleep: slow-wave sleep (non-rapid eye movement sleep) and rapid eye movement sleep (REM sleep). Sleep is a state of physiological loss of consciousness from which a subject can be aroused by appropriate stimuli.
Phases of sleep
During sleep, a subject passes periodically through several stages in an orderly fashion. These stages are defined by the appearance of certain wave patterns in the EEG.
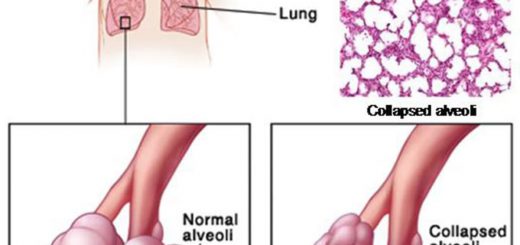
A. Slow-wave sleep (non-REM sleep): this type of sleep is characterized by:
- A drop of blood pressure (10-30%).
- Decrease of heart rate– decrease in the peripheral vascular tone.
- Decrease in the respiratory rate.
- Decrease of the basal metabolic rate.
- Increase growth hormone secretion during stages 3 and 4.
- Dreams do occur but they are not consolidated, therefore not remembered.
Stages of slow-wave sleep
Slow-wave sleep (non-REM sleep) is divided into 4 stages depending upon EEG pattern. During wakefulness with closed eyes and a relaxed mind, the alpha waves of EEG appear, The passage from wakefulness to non-REM sleep is characterized by progressively slower frequencies and higher voltage activities in the EEG.
Non-REM sleep comprises four stages:
- Stage I: theta waves start to appear.
- Stage II: is characterized by sleep spindles superimposed on the theta waves.
- Stage Ill: EEG starts to show slower delta waves.
- Stage IV: stage of deep sleep, delta waves become more prominent with low frequency & high amplitude.
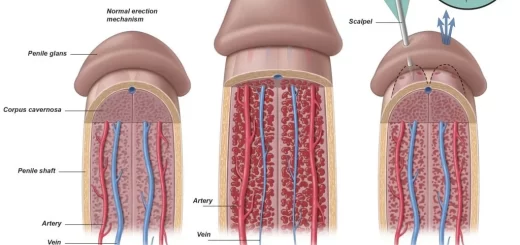
B. Rapid eye movement sleep (REM sleep): this type occurs in episodes of 5-30 minutes which recur about every 90 minutes. It is characterized by:
- An irregular heart and respiratory rate. Some autonomic reactions frequently occur in REM sleep including penile erection in males and inhibition of gastrointestinal activity.
- It is associated with active dreaming that is later remembered.
- There is a reduction in homeostatic mechanisms such as a decrease in the response of the respiratory system to changes in blood CO2.
- Muscle tone is markedly decreased especially (hypotonia).
- The eyes show rapid back-and-forth movements.
- EEG shows activity similar to the waking state showing low voltage rapid waves very similar to the beta rhythm of the EEG during arousal.
Sleep-wake cycle
The sleep cycle consists of one episode of non-REM followed by REM sleep, This cycle is repeated 4-6 times every night, A young adult first enters non-REM sleep, passes through stage 1 and 2, and spend 70-100 minutes in stage 3 and 4, then sleep lighten again, ascend to stage 2 and suddenly enters a brief period of REM sleep, This cycle is repeated at intervals of about 90 minutes throughout the night. However, there is less stage 3 and 4 sleep and more REM sleep toward morning.
Upper and lower motor neurons lesion, Stages of complete spinal cord transection
Diencephalon function, Thalamus, Metathalamus, Hypothalamus, Epithalamus and Subthalamus
Function and Physiology of Thalamus, hypothalamus and Limbic system