Pathogenesis of bacterial infection, Classification of Pathogens and Bacterial virulence factors
Bacterial infection is due to the disturbance in the balance between bacterial virulence and host resistance, The objective of bacteria is to multiply rather than to cause disease; and it is in the best interest of the bacteria not to kill the host.
Pathogenesis of bacterial infection
We live in an environment that favors the microbe because the growth rate of bacteria far exceeds that of most eukaryotic cells, The human body carries 10 times more bacteria than human cells, and only 50/103 of bacterial species we carry cause disease.
Important definitions
- Microbiota: Microbial flora harbored by normal, healthy individuals.
- Adherence: The process by which bacteria stick to the surfaces of host cells, After bacteria have entered the body, adherence is a major initial step in the infection process, The terms adherence, adhesion, and attachment are often used interchangeably.
- Colonization: colonization is the presence of multiplying bacteria on a body surface (like on the skin, mouth, intestines or airways) without causing disease in the person.
- Infection: Invasion and Multiplication of an infectious agent within the body.
- Invasion: The process whereby bacteria enter host cells or tissues and spread in the body.
Normal Human Microbiota
The normal microbiota denotes the population of microorganisms that inhabit the skin and mucous membranes of healthy normal persons, The normal microbiota provides the first line of defense against microbial pathogens, assists in digestion, and contributes to the maturation of the immune system, The skin, and mucous membranes always harbor a variety of microorganisms that can be divided into:
- Resident microbiota, which are fixed types of microorganisms regularly found in a given area at a given age that, if disturbed, promptly reestablish themselves.
- Transient microbiota, which are nonpathogenic or potentially pathogenic microorganisms that inhabit the skin or mucous membranes for hours, days, or weeks.
Classification of Pathogens
Pathogens can be classified as primary pathogens or opportunistic pathogens.
- The primary pathogen can cause disease in a normal healthy host regardless of the host’s resident microbiota or immune system, Its presence is abnormal, Examples include Mycobacterium tuberculosis (tuberculosis) and Yersinia pestis (plague).
- Opportunistic pathogen: can only cause disease in situations that compromise the host’s defenses, such as the body’s protective barriers, immune system, or normal microbiota, Other members of the normal microbiota can also cause opportunistic infections when microbes that reside harmlessly in one body location end up in a different body system.
Individuals susceptible to opportunistic infections include the elderly, patients undergoing chemotherapy, people with immunodeficiencies (e.g. AIDS), and patients who have had a breach of protective barriers (such as a severe wound or burn). Examples:
- Staphylococcus epidermidis is a member of the normal microbiota of the skin, where it is generally avirulent. However, in hospitals, it can also grow in biofilms that form on catheters, implants, or other devices that are inserted into the body during surgical procedures, Once inside the body. S. epidermidis can cause serious infections such as prosthetic valve endocarditis.
- E.coli normally found in the large intestine can cause a urinary tract infection If it enters the urinary tract.
- viridans Streptococci may produce infective endocarditis in a previously damaged heart valve (by congenital disease or rheumatic fever), if the organism reaches the bloodstream after tooth extraction or tonsillectomy.
- Other bacteria only cause disease in immunosuppressed and debilitated persons and are opportunistic pathogens. (e g. Pseudomonas species).
Infectious process
The infectivity of the pathogen (capacity to initiate infection) is related to:
- Dose of the pathogen (the infective dose); the number of bacteria required to cause disease.
- Its growth phase (bacteria are more infective in the log phase than the lag phase.
- Its virulence.
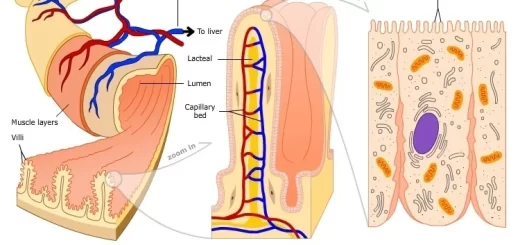
The pathogen should be able to gain entry to the host, travel to the location where it can establish an infection, evade or overcome the host’s immune response, and cause damage (ie., disease) to the host, In the body, most bacteria cause infection first by attaching or adhering to host cells, usually epithelial cells.
After the bacteria have established a primary site of infection, they multiply and spread directly through tissues or via the lymphatic system to the bloodstream, This allows bacteria to spread widely in the body and permits them to reach tissues particularly suitable for their multiplication.
Bacterial virulence factors
Many factors determine bacterial virulence or the ability to cause infection and disease, These factors help the microorganisms to invade the host, evade host defenses, and cause disease, The following are types of virulence factors:
- Adherence factors.
- Invasion.
- Antiphagocytic factors.
- Toxin production.
- Extracellular enzymes.
- Bacterial biofilms.
- Intracellular survival.
Adherence factors
Certain bacteria have specialized structures e.g.pili, that help their adherence to the host cell mucous membranes thus allow them to start the disease process, If they do not adhere, they will be swept away e.g. E. coli has pili to mediate the attachment to urinary tract epithelium, The lipoteichoic acid cause adherence of the streptococci to buccal epithelial cells.
Invasion
It is the ability of bacteria to invade the tissue and multiply, Invasion of the host’s epithelium is central to the infectious process.
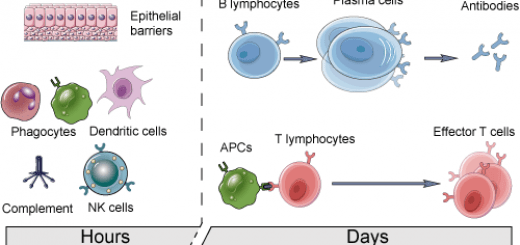
Antiphagocytic Factors
Some pathogens evade phagocytosis or leukocyte microbicidal mechanisms by adsorbing normal host components to their surfaces, For example, Staphylococcus aureus has surface protein A, which binds to the Fc portion of IgG, Other pathogens have polysaccharide capsules that impede phagocytosis (e.g., S. pneumoniae and N. meningitidis), S. pyogenes has M protein.
Toxin production
Toxins produced by bacteria are generally classified into two groups: endotoxin (LPS), which is present in the outer membrane of Gram-negative rods, and exotoxins which are secreted by bacterial cells.
Extracellular enzymes
These are produced by pathogens to play important roles in the infectious process. Example: Staphylococcus aureus produces coagulase, which works in conjunction with blood factors to coagulate plasma, Coagulase contributes to the formation of fibrin walls around staphylococcal lesions, which helps them persist in tissues, Hyaluronidases are enzymes that hydrolyze hyaluronic acid, a constituent of the ground substance of connective tissue (e.g., staphylococci, streptococci). IgA proteases destruct mucosal IgA secreted by Neisseria meningitidis, Haemophilus influenzae, and Streptococcus pneumoniae.
Bacterial biofilms
A biofilm is an aggregate of interactive bacteria attached to a solid surface or to each other and encased in an exopolysaccharide matrix, A single species of bacteria may be involved or more than one species may coaggregate to form a biofilm, The bacteria in the exopolysaccharide matrix may be protected from the host’s immune mechanisms, This matrix also functions as a diffusion barrier for some antimicrobials, Biofilms are important in human infections that are persistent and difficult to treat (e.g. Staphylococcus epidermidis of central venous catheters, prosthetic infections).
Intracellular survival
Some bacteria (eg, Mycobacterium tuberculosis) live and grow intracellular within polymorphonuclear cells, macrophages, or monocytes, Evading intracellular killing by phagocytic cells can be accomplished by several mechanisms: they may avoid entry into the phagolysosomes and live within the cytosol of the phagocyte; they may prevent the phagosome-lysosome fusion and live within the phagosome, or they may be resistant to lysosomal enzymes and survive within the phagolysosome.
Transmission of infection
Bacteria can adapt to a variety of environments that include external sources such as soil, water, and organic matter or internal milieu as found within insect vectors, animals, and humans, where they normally reside (reservoir of infection).
An anatomic site through which pathogens can pass into host tissue is called a portal of entry, The most frequent portals of entry of pathogenic bacteria into the body are the sites where mucous membranes meet with the skin, which are the respiratory (upper and lower airways), gastrointestinal (primarily mouth), genital, and urinary tracts.
Pathogens may also enter the body through a breach in the protective barriers of the skin and mucous membranes (e.g., wounds, insect bites, animal bites, needle pricks), There must be a mode of transmission of bacteria to a new host. Different modes of transmission include the following:
1. Contact transmission includes direct contact or indirect contact.
- Direct contact can be categorized as vertical (mother to child) horizontal (touching. kissing, sexual), or droplet transmission, When an individual coughs or sneezes, small droplets of mucus that may contain pathogens are ejected. This leads to direct droplet transmission of a pathogen to a new host over distances of one meter or less (e.g. Influenza viruses).
- Indirect contact transmission involves inanimate objects called fomites that become contaminated by pathogens from an infected individual or reservoir, Transmission occurs indirectly when a new susceptible host later touches the fomite and transfers the contaminated material to a susceptible portal of entry.
2. Vehicle Transmission
The term vehicle transmission refers to the transmission of pathogens through vehicles such as water, food, and air. Airborne transmission is the transmission of pathogens through droplet nuclei (< 5 microns); unlike larger particles that drop quickly out of the air column, fine droplets produced by coughs or sneezes can remain suspended for long periods, traveling considerable distances (e.g. Mycobacterium tuberculosis).
3. Vector Transmission
Diseases can also be transmitted by a mechanical or biological vector (typically an arthropod) that carries the disease from one host to another, Mechanical transmission is facilitated by a vector that carries the pathogen from one host to another without being infected itself (e.g. cases of diarrhea).
For the pathogen to persist, it must put itself in a position to be transmitted to a new host, leaving the infected host through a portal of exit, Similar to portals of entry, the most common portals of exit include the skin and the respiratory, urogenital, and gastrointestinal tracts.
Characteristics of Exotoxins and Endotoxins
Exotoxins
They are excreted by living bacterial cells, They are produced by both Gram +ve and Gram -ve bacteria, They are polypeptides, They are relatively unstable; toxicity is destroyed rapidly by heating at a temperature above 60 °C, They are converted to antigenic, non-toxic toxoids by chemicals or heat (e.g. tetanus toxoid), they usually bind to specific receptors on host cells and exerts a specific action, Exotoxins may be subclassified as enterotoxins, neurotoxins or cytotoxins.
Endotoxins
They are integral parts of the cell wall of Gram-negative bacteria. They are released upon bacterial death, They are found only in Gram-ve bacteria, They are Lipopolysaccharide (LPS) complex, They are relatively stable, withstand heating at a temperature above 60 °C for hours without loss of toxicity, and they are not converted to toxoids.
Specific receptors not found on host cells, LPS activates macrophages and neutrophils, Pro-inflammatory cytokines, such as IL 1-, IL6-, IL8-, TNF-α, and other cytokines, are released, and the complement and coagulation cascades are activated, The following can be observed clinically: fever, leukopenia, and hypoglycemia; hypotension and shock resulting in impaired perfusion of essential organs (eg, brain, heart, and kidney); intravascular coagulation; and death, from massive organ dysfunction.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Features and classification of viruses, Defective viruses and Viral vectors used for gene therapy
Bacterial growth phases and Environmental factors required for bacterial growth
Microbiology, Bacteria structure, types, Gram-positive bacteria & Gram-negative bacteria