Hepatorenal syndrome (HRS) risk factors, diagnosis, symptoms, types, causes and treatment
Hepatorenal syndrome (HRS) is the development of renal failure in patients with severe liver disease (acute or chronic) in the absence of any other identifiable causes of renal pathology. HRS is a common but severe complication in cirrhotic patients with ascites. About 20% of cirrhotic patients with ascites and normal renal function develop the syndrome after 1 year of follow-up, and 39% at 5 years.
Risk factors of HRS
- GI bleeding.
- Excessive diuresis.
- Inexpert paracentesis.
- Electrolyte imbalance (severe diarrhea).
- Infections.
- SEP
- Nephrotoxic drugs (NSAIDs, aspirin, aminoglycosides, iodine-containing contrast agents, and cyclosporine).
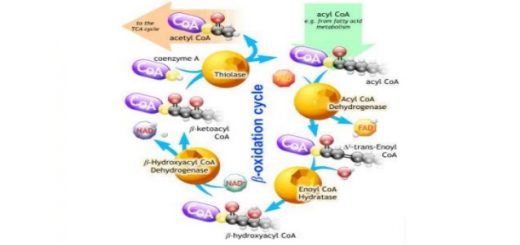
Pathogenesis
HRS has been considered a functional rather than structural disturbance in renal function. However, an additional structural component has been suggested due to systemic inflammatory response syndrome secondary to bacterial translocation from the gut leading to the production of pro-inflammatory cytokines, which enhance the release of nitric oxide and subsequently splanchnic arterial vasodilatation.
HRS is mainly related to splanchnic arterial vasodilatation mediated by the accumulation of endogenous vasodilators. In advanced cirrhosis, splanchnic arterial vasodilation becomes very severe and leads to a marked decrease in systemic vascular resistance and severe arterial underfilling.
Subsequently, activation of endogenous vasoconstriction factors, RAAS, SNS and ADH release results in marked renal vasoconstriction, When the local renal vasodilators (nitric oxide, prostaglandins and Kallikrein-kinin system) are not able to counterbalance the effects of the vasoconstrictor neurohormonal system (endothelin-1, Thromboxane A2 and Leukotriene and glomerular E4), severe decrease filtration rate occurs in renal blood flow associated with corticomedullary shunting leading to the development of HRS.
Manifestations
1. History
- Usually non-specific symptoms, such as anorexia, weakness, and fatigue.
- HRS is usually noticed with decreased urine output and when blood test results show a decline in renal function.
- In the later stages, nausea, vomiting and thirst occur, The patient is drowsy.
- Progressive azotemia is usually with hepatic failure and ascites which is difficult to control.
2. Physical examination
- Reflects the advanced liver disease: (hepatosplenomegaly, ascites, PHTN stigmas, asterixis, scleral icterus, gynecomastia, coagulopathies, palmar erythema, spider nevi, constitutional disorders such as weakness, fatigue, anorexia, etc.).
- Presence of circulatory abnormalities (low mean arterial blood pressure (MAP)<80 mmHg, tachycardia, bounding pulse).
Diagnosis
Major Criteria
- Severe cirrhosis with ascites.
- Rise in serum creatinine by 0.3 mg/dl in < 48 hour or a rise of serum creatinine ≥ 50% from baseline.
- Absence of shock, ongoing bacterial infection, and current or recent treatment with nephrotoxic drugs, absence of Gl fluid loss.
- No sustained improvement in renal function despite the optimization of volemia (by stopping diuretics and infusing albumin or 1.5 L of isotonic saline).
- Proteinuria below 0.5 g/l, no ultrasonographic evidence of renal obstructive disease.
Additional criteria
- Urine volume < 500 ml/ day.
- Urine osmolality > plasma osmolality.
- Urine sodium < 10 mmol/day.
- Urine RBCs < 50/HPF (high power field).
- Serum sodium <130 mmol/L.
Classification
HRS-acute kidney injury (AKI) (formerly Type-1 HRS):
- Rapidly progressive reduction of renal function (AKI) (over days to weeks).
- Rise in serum creatinine by <0.3 mg/dl in <48 hours or a rise of serum creatinine ≥ 50% from baseline.
- Complication of SBP.
HRS-chronic kidney disease (CKD) (formerly Type-2 HRS):
- Slowly progressive (over months).
- GFR of < 60 ml/min for > 3 months using the Modification of Diet in Renal Disease (MDRD) equation.
- Associated with refractory ascites.
Prognosis of HRS
- Without treatment, there is an 80% mortality at 2 weeks in HRS, with only 10% surviving more than 3 months.
- New pharmacological approaches to reversing or stabilizing renal dysfunction may improve survival.
Differential diagnosis of HRS
- Prerenal azotemia from volume depletion & Postrenal azotemia from outflow obstruction.
- Acute tubular necrosis & Renal vascular disease & Alcohol-related renal disease.
- Glomerular mesangial IgA deposits complicate cirrhosis.
- Immune-related glomerulonephritis due to Hepatitis B and C.
Prevention
- Careful use and monitoring of diuretic therapy, nephrotoxic drugs are avoided.
- Early recognition of any complication such as electrolyte imbalance, hemorrhage or infection.
- Tense ascites may be drained to improve renal hemodynamics by decreasing IVC and renal vein pressure.
- Administration of salt-poor albumin after total volume paracentesis and spontaneous bacterial peritonitis (SBP) (volume expansion, removing cytokines and bacterial products).
- Prophylactic antibiotics in patients already having one episode of SBP.
Treatment
General measures
- Stop diuretics & Beta blockers.
- Monitor fluid overload is necessary.
- Exclude other causes of renal failure.
- Identify condition.
- Plasma expansion with albumin solution; search for sepsis and SBP s that may be reversible.
- A broad-spectrum antibiotic is started irrespective of proof of infection.
- Intravenous N-acetylcysteine.
Pharmacological treatment
- Systemic vasoconstrictors are used in conjunction with albumin infusion as the first-line treatment.
- The most commonly used vasoconstrictors are vasopressin analogues (Terlipressin or Glypressio) 0.5-2 mg/4h intravenous, somatostatin analog (octreotide) 25-50 mcg/h intravenous infusion, and oral alpha-adrenergic agonists (midodrine) for 5-15 days.
TIPS
- It may improve renal perfusion and reduce the activity of the RAAS.
- TIPS is used when medical management fails, as a bridge to liver transplantation.
Hemodialysis (renal replacement therapy)
- It is not considered effective.
- Continuous arteriovenous and venovenous hemofiltration have been used but not formally evaluated.
Liver transplantation
- It is the definitive treatment) for HRS.
- The use of vasoconstrictors and albumin may improve renal dysfunction and allow elective transplantation.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Spontaneous bacterial peritonitis symptoms, diagnosis, treatment, causes and antibiotics
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Liver Cirrhosis causes, symptoms, treatment & stages, Liver Biopsy and treatment of PHTN
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Liver development, congenital anomalies, function & Pancreas development