Blood transfusion causes, Haemolytic transfusion reaction & Acute renal failure
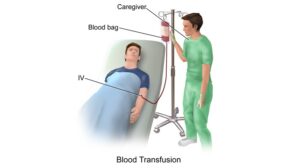
The people receive blood transfusions for many reasons such as surgery, injury, disease & bleeding disorders, Blood transfusion is a medical procedure in which donated blood is provided to you through a narrow tube placed within a vein in your arm, This life-saving procedure helps replace blood lost due to surgery or injury. Blood transfusion can help if an illness prevents your body from making blood or some of your blood’s components correctly.
Blood transfusion
Blood transfusion is used for many medical conditions, It is the process of transferring blood or blood products into one’s circulation intravenously, It is used to replace lost components of the blood, modern medical transfusions uses only components of the blood, such as red blood cells, white blood cells, plasma, clotting factors, and platelets.
Red blood cells (RBC) contain hemoglobin and supply the cells of the body with oxygen, White blood cells are not used during transfusion, but are part of the immune system, and fight infections, Plasma is the liquid part of the blood, It acts as a buffer, and contains proteins and important substances needed for the body’s overall health, Platelets are used in blood clotting, and they prevent the body from bleeding.
Blood transfusions occur without complications. When complications do occur, they’re typically mild. In 1818, British obstetrician James Blundell successfully transfused human blood for the first time, to a patient who had bled during childbirth. Subsequently, several blood transfusions were done: some saved lives, while others ended in severe complications and death.
The reason behind the often fatal blood transfusions became clear when Karl Landsteiner, an Austrian physician, discovered the first 3 human blood groups, A, B, and C in 1900. Blood type C was later changed to O. He received the Nobel Prize for physiology or Medicine in 1930. His colleagues Alfred Decastello and Adriano Sturli added AB, the fourth type, in 1902.
Why Would You Need a Blood Transfusion?
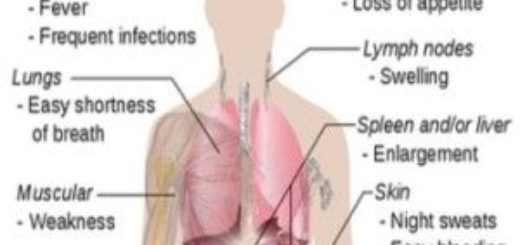
When you’ve had major surgery or a serious injury and you need to replace lost blood, If you’ve experienced bleeding in your digestive tract from an ulcer or other condition, If you have a blood disorder or severe liver problems, When you have an illness such as leukemia or kidney disease that causes anemia (not enough healthy red blood cells), when you’ve received cancer treatments like radiation or chemotherapy.
Indications of blood transfusion
- Circulatory shock: loss of large amounts of blood e.g. haemorrhage causes a severe drop of arterial blood pressure.
- Severe anemia.
- Severe leukopenia.
- Haemorrhagic diseases: Deficiency of some coagulation factors as in haemophilia or decrease of blood platelets count below 50.000 cell/cmm as in thrombocytopenic purpose.
Transfusion of blood components
Several components of blood can be isolated and transfused alone, such as:
- Fresh frozen plasma infusion can be used for reversal of anticoagulant effects like warafin, or to supply coagulation factors on known coagulation factor deficiency (e.g. haemophilia).
- Platelet transfusion is indicated to prevent haemorrhage in patients with severe thrombocytopenia or platelet function defects.
- Red cell transfusion can be used for the correction of intractable anemia by supplying RBCs without causing volume overload.
Steps have done before blood transfusion
- Determination of ABO and Rh blood groups.
- Cross-matching.
Cross-matching
In cross-matching, donor red cells are mixed with recipient plasma on a slide and checked for agglutination. It is advisable to check the action of the donor’s plasma on the recipient cells in addition, even though, as noted above, this is rarely a source of trouble. If agglutination occurs in any one of the two slides or both, then these types of blood are not compatible and blood transfusion should not be performed.
The aim of this procedure is to detect the presence of any possible unknown agglutinogens that would cause transfusion reactions due to incompatibilities in systems other than ABO and Rh. Thus blood should never be transfused without being across matched except in the most extreme emergencies.
Transfusion reactions resulting from mismatched transfusion
Haemolytic transfusion reaction
When one type of blood is transfused to a recipient of an incompatible blood type, a haemolytic transfusion reaction is likely to occur as the red blood cells of the donor blood are agglutinated, haemolysed then phagocytosed by the tissue macrophage system where hemoglobin is released.
Fate of released hemoglobin: Hemoglobin released from the red cells is converted by phagocytes into bilirubin that is excreted into the bile by the liver. The concentration of bilirubin in the body fluid rises high enough to cause jaundice, i.e the person’s tissues become tinged with yellow bile pigments. Some of free hemoglobin can leak through the glomerular membranes into the kidney tubules leading to acute renal failure.
Acute renal failure
One of the most fatal effects of transfusion reactions is acute kidney failure that seems to result from three different causes:
- Renal ischemia: The haemolysedcells release toxic substance that can cause powerful renal vasoconstriction leading to renal ischemia.
- Circulatory shock: The loss of circulating red blood cells of the recipient along with the production of toxic substances from hemolysed cells (e.g. histamine) can cause a severe drop of ABP. thus, the renal blood flow and urinary output decrease leading to circulatory shock.
- Blocking of renal tubules: If the total amount of free hemoglobin in the circulation is greater than that which bind with haptoglobin (a plasma protein that can bind small amounts of hemoglobin) much of it leaks through the glomerular membranes into the renal tubules blocking some of them.
All these factors can lead to acute renal failure and if the failure is complete, the patient may die within a weak or two unless properly treated.
Autologous transfusion
In order to eliminate the risk of transfusion reactions and prevent the transmission of infectious blood-borne diseases, autologous transfusion is sometimes done. In this popular procedure, the withdrawal of the patient’s own blood in advance of elective surgery is done. Then, it is infused back to the same patient during the surgery if needed.
Blood groups, Rh blood groups, Erythroblastosis fetalis & Importance of Rh factor
Blood constituents & Physical properties, Sources & functions of plasma proteins
Red blood cells (Erythrocytes) structure & function, Myeloid tissue & Bone marrow
Anemias causes, symptoms, features, diagnosis & Types of Polycythemia
Functions and sources of Folic acid, Cobalamin (vitamin B12) & Vitamin K
Factors that help iron absorption, Daily iron requirements & Abnormal iron levels
Platelets definition, function, structure, normal range & Thrombopoiesis