Idiopathic Inflammatory Myopathies definition, symptoms and treatment
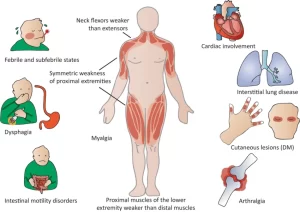
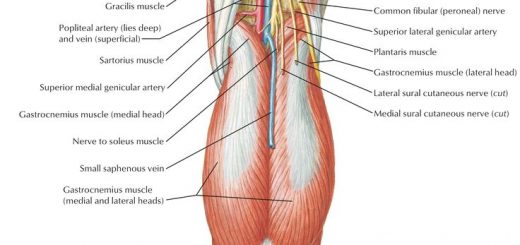
Idiopathic inflammatory myopathy is characterized by inflammation of the muscles used for movement (skeletal muscles), The primary symptom is muscle weakness, which develops gradually over a period of weeks to months or years, Other symptoms include joint pain and general tiredness (fatigue).
Idiopathic Inflammatory Myopathies
Idiopathic Inflammatory Myopathies are a heterogeneous group of disorders characterized by: Proximal muscle weakness and non-suppurative inflammation of skeletal muscle with predominantly lymphocytic infiltrates. Idiopathic inflammatory myopathies are characterized by inflammation of muscles (myositis) and other body systems, The diagnosis can be challenging because of the many potential clinical features and extra-muscular manifestations.
Epidemiology
- 2-8 cases per million per year.
- Female: male= 2:1
- Bimodal distribution (2 age groups): 7-10 years. 45-60 years.
- The age of onset for myositis associated with another condition is similar to that in the other condition.
- IBM (Inclusion body myositis) and Myositis associated with malignancy are common after the age of 50 years.
Pathogenesis
The etiology of IIM is unknown. Aberrations (Abnormalities) in the immune system give rise to an increased susceptibility to infectious agents. Also Genetic and Environmental factors. Modifications of cellular immunity that lead to the development of mononuclear cells capable of injuring muscle. Complement may play a role in tissue injury.
Polymyositis
In polymyositis, “myos-” refers to the muscles, “poly-” means many, and “-itis” refers to inflammation, so polymyositis is an inflammatory disorder that involves many muscle groups around the body. Polymyositis is an immune-mediated disease, meaning that the immune system attacks muscles in our own body.
Pathogenesis
Healthy muscle cells present normal muscle proteins on the MHC class I molecule, and the cytotoxic T-cells inappropriately react and get activated.
That’s because it’s thought that the muscle proteins might look similar to a foreign pathogen. This is called molecular mimicry, because from the perspective of the cytotoxic T-cell, a host protein is mimicking a foreign protein. When the cytotoxic T-cells are activated by the autoantigen, they cause apoptosis of the muscle cells. B-cells start producing antibodies against these autoantigens as well.
The immune reaction causes inflammation in and around the muscles that are being attacked by the immune response, and typically these attacks occur repeatedly over time and can involve different muscle groups.
Clinical picture
Dermatomyositis
In dermatomyositis, “-itis” refers to inflammation, “myos-” to the muscles, and “dermato-” to the skin, so dermatomyositis is an inflammatory disorder that involves both the skin and the muscles, Dermatomyositis is considered to be an autoimmune disease, meaning that the immune system attacks the cells in our own body.
Pathogenesis
The exact trigger for dermatomyositis is unknown, but there are some specific genetic and environmental factors
Genetic factors: HLA-DR3 or HLA-DR5 + Environmental factors: Exposed to a foreign pathogen like coxsackievirus or specific tumor antigens, such as those in ovarian, lung or breast tumors.
Immune cells confuse normal muscle and skin proteins with foreign antigens. (molecular mimicry) → Autoantigens are usually found in the endothelial cells lining the capillaries in muscle and skin cells, as well as soluble antigens coming from the nucleus or cytoplasm of destroyed muscle cells and skin cells → Loss of skin and muscle cells
Characteristics
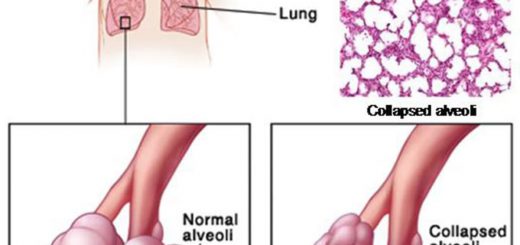
The rash is the primary presenting feature in 95%. Only 50% to 60% of patients have proximal muscle weakness at presentation. Follow-up of patients with a rash is therefore essential, as most eventually manifest proximal weakness (If no weakness develops, this leads to a Subgroup: Amyopathic DM). Arthralgia, Raynaud’s phenomenon, and dysphagia are seen in 10% to 25% of DM patients. Rarely interstitial pneumonitis, cardiomyopathy, and heart block.
Skin in Dermatomyositis
- Heliotrope rash: Violaceous discoloration of eyelids, often associated with peri-orbital edema (Peri-orbit = Eyelids).
- Shawl sign: Macular Erythema over the posterior shoulders and chest.
- Mechanic’s Hands: Dark or Dirty appearing horizontal lines over palmar and lateral aspects of fingers.
- V sign: Macular Erythema over anterior neck and upper chest.
- Gottron’s sign/papules: Symmetric, Scaly, Violaceous or Erythematous, macular or raised eruption over extensor surfaces of MCP and IP joints, elbows, knees, medial malleoli.
Diagnosis of PM & DM
- Symmetric, progressive proximal muscle weakness.
- Elevation of serum levels of muscle-associated enzymes: Creatinine Kinase, Aldolase, LDH, and AST.
- Typical Electromyographic triad.
- Evidence of chronic inflammation in muscle biopsy.
- Characteristic rashes of Dermatomyositis
- To diagnose PM FIRST 4 CRITERIA must be present.
- To diagnose DM LAST CRITERION + 3 OTHER CRITERIA must be present.
Childhood (Juvenile) myositis
- Childhood DM-PM appears most commonly between ages 7 and 10 years.
- Slightly more often in girls than in boys.
- Most have the characteristic rash of DM at presentation.
- About 90% present with proximal muscle weakness.
- Distinctive features of the myopathy are atrophy, contractures, and tissue calcifications.
- Visceral involvement is more frequent than in the adult form: (Abnormal pulmonary Function, Esophageal motility, and Gastrointestinal absorption).
- Some may present with acute myositis with Fever, Malaise, and Abdominal pain.
- Gastrointestinal ulcerations caused by diffuse necrotizing arteritis may occur and lead to hemorrhage.
Myositis with Connective Tissue Diseases
Overlap syndromes as defined here consist of PM or DM that fulfills the previously mentioned criteria and another connective tissue disease that fulfills a separate set of diagnostic criteria. The presenting features reflect the underlying connective tissue disease.
Myositis with Malignancy
- The possibility of malignancy in an elderly patient with PM-DM is FOUR times greater than in an age-matched control.
- Between 10% and 20% of patients with PM-DM may have an underlying malignancy.
- DM has a higher association with malignancy than does PM (DM > PM).
- Myositis precedes malignancy by an average of 1 to 2 years in 70% of patients and follows it in 30%.
Inclusion Body Myositis
Inclusion body myositis (belongs to a group of muscle diseases known as inclusion body myopathies characterized by the presence of vacuoles and inclusions formed by clumps of protein that collect within the muscle fibers.
Pathogenesis
The exact mechanism is unclear, but one thought is that the trigger may be a virus that infects and damages myocytes.
The virus infects and damages myocytes →In response, the muscle cells start to present the antigens on their MHC class I proteins → The rough endoplasmic reticulum of the myocytes fill up with these MHC class I proteins, and some begin to misfold → The misfolded proteins begin to aggregate and that causes additional degeneration and destruction of muscle fibers.
Symptoms
Symptoms begin insidiously and differ from Palymyositis in that IBM
- May include focal distal or asymmetric weakness.
- Only borderline elevation of enzymes.
- Neurogenic or Mixed Neurogenic / Myopathic changes on EMG.
- Poor response to therapy.
- Symptoms may continue to progress slowly & steadily: in others, symptoms plateau.
Investigations
Acute phase reactants (ESR and CRP): ESR is normal in 50%.
Anti-Nuclear Antibody (ANA): It may be positive in over 50% of patients with IIM. It may be in low titer and are non-specific in nature. The presence of a high titer may indicate an associated CTD (Such as: SLE).
Muscle enzymes: Elevation of CK sometimes during the course of the disease (Often >10 times the normal). AST, ALT, Aldolase and LDH are elevated in most cases.
EMG (Electromyography) Findings: EMG classically reveals the following triad (In PM and DM):
- Increased insertional activity, fibrillations, and sharp positive waves.
- Spontaneous, bizarre, high-frequency discharges.
- Polyphasic motor-unit potentials of low amplitude and short duration.
Complete triad is seen in 40% of patients. 10-15 % of patients have completely normal EMGs. An incomplete triad may also be present.
Treatment
- The majority of IIM patients improve with corticosteroid treatment.
- However, immunosuppressive agents are both steroid-sparing and effective in treating serious extra-muscular manifestations.
- MTX is first-line therapy after corticosteroids in steroid-refractory myositis.
- Studies demonstrate the effectiveness of azathioprine in myositis.
- The combination of azathioprine and MTX proved efficacious when either agent is ineffective alone.
Others:
- Cyclosporine and Tacrolimus.
- Intravenous Immunoglobulin (IV Ig).
- Mycophenolate Mofetil.
Following up:
- Regaining muscle power.
- Decreased muscle-associated enzymes.
- Pulmonary function tests.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Systemic Lupus Erythematosus symptoms, diagnosis, types and treatment
Rheumatoid Arthritis (RA) causes, stages, symptoms, diagnosis, and specific joint affection
Rheumatoid Arthritis diagnosis and treatment, Disease-Modifying antirheumatic drugs (DMARDs)
Non-radiographic axial spondyloarthritis, Reactive arthritis, and Enteropathic arthritis