Testis functions, sperms production, Factors affecting spermatogenesis and Structure of Epididymis
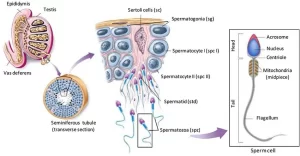
Spermatogenesis (formation of spermatozoa) is a process by which the male germ cells are transformed into spermatozoa. Spermatogenesis occurs in the seminiferous tubules during active sexual life, under the stimulatory effects of the anterior pituitary gonadotropic hormones. It begins at an average age of 13 years and continues throughout the remainder of life but decreases markedly in old age.
Histological features of spermatogenesis
The process of spermatogenesis is divided into 2 phases:
- Spermatocytogenesis: spermatogenic cells undergo successive mitotic and meiotic divisions to give rise to spermatids.
- Spermiogenesis: spermatids undergo morphological changes to be differentiated into spermatozoa. All these changes occur while spermatids are embedded in the luminal surface of Sertoli cells.
Histological structure of mature spermatozoon
At the end of spermiogenesis, the mature sperm is formed of head, neck, and tail and surrounded by the cell membrane.
- Head of the sperm: It is flattened with an acrosomal cap containing the hydrolytic enzymes, mainly hyaluronidase, to dissociate the cells of corona radiata and digest the zona pellucida around the ovum during fertilization (acrosomal reaction). It contains a dense homogeneous nucleus, having 23 s-chromosomes
- Neck (connecting piece): this contains the centrioles, from one of them the tail of the sperm is formed during spermiogenesis.
- Tail (sperm flagellum); this is subdivided into:
1. Middle piece: extends from the neck to the annulus (a ring-like dense material at the cell membrane, found at the end of the middle piece). It consists of:
- The axoneme of the flagellum.
- 9 outer dense fibers, each is laying outer and opposite to the 9 doublets of the axomene.
- Mitochondrial sheath formed of spirally-arranged mitochondria to provide energy for motility of sperm tail.
2. Principal piece: extends from the annulus to the end piece. It consists of
- The axoneme.
- 7 outer dense fibers.
- The fibrous sheath, is present outside the outer dense fibers and is formed of circumferential ribs of dense material joined together by the ventral and dorsal longitudinal columns.
3. End piece: it consists of the axoneme covered by the flagellar membrane (sperm cell membrane).
Factors affecting spermatogenesis
(I) Hormones
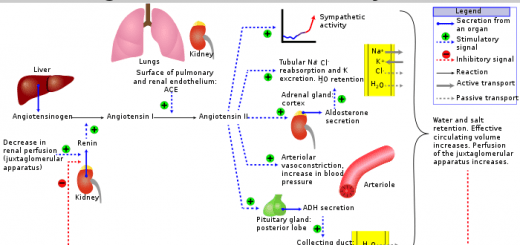
A- Anterior gonadotrophic hormones (GnTHs):
I. FSH: FSH stimulates spermatogenesis and Sertoli cell function. It also maintains a high concentration of testosterone in the seminiferous tubular fluid by:
- Promoting secretion of the ABP from the Sertoli cells.
- Sensitization of Leydig cells to the action of LH.
2. LH: This stimulates testosterone secretion from the interstitial cells of Leydig (so it is called the interstitial cell-stimulating hormone or ICSH).
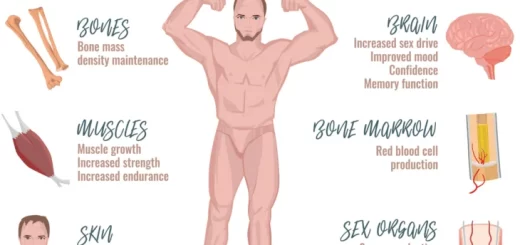
B- Testosterone: it is secreted from the Leydig cells under the effect of LH and it reaches the seminiferous tubules directly where it is maintained at a high concentration by the effect of the ABP. It is essential for the division of the germinal cells. It stimulates the meiotic division of the primary spermatocyte to form a secondary spermatocyte. It is also essential for the maturation phase of spermatogenesis particularly spermatid maturation in the Sertoli cell.
Administration of exogenous androgens in large doses inhibits LH secretion, so the secretion of endogenous androgen by the Leydig cells is decreased. This decreases the local androgen concentration in the testes resulting in depression or spermatogenesis, so treatment with exogenous androgens can be used as a method of contraception in males.
C- Other hormones:
- Estrogens formed from testosterone by the Sertoli cells when they are stimulated by follicle-stimulating hormone, are probably also essential for spermiogenesis, Inhibin depresses spermatogenesis by inhibiting FSH secretion.
- Thyroxine stimulates spermatogenesis, so it is depressed in cases of myxedema.
- Growth hormone and most of the other hormones: For controlling metabolic functions of the testes, GH specifically promotes early division of the spermatogonia, In its absence, spermatogenesis is severely deficient or entirely absent.
(2) Temperature
Spermatogenesis requires a lower temperature than that of the body (optimally 32-33 °C). Rise of the testicular temperature e g. due to cryptorchidism, fevers, or continuous wearing of tight pants, damages the germinal epithelium (thus inhibiting spermatogenesis) and may kill any preformed sperms resulting in infertility.
Spermatogenesis is also depressed at lower temperatures than 32 °C. For this reason, the dartos muscle contracts in cold weather to draw the testes upwards (in order to be warmed by the abdominal temperature).
Failure of descent of the testes into the scrotum is known as cryptorchidism, this will maintain the testis at 37°C which damages the germinal epithelium and disturbs spermatogenesis leading to sterility. However, the interstitial cells of Leydig are not affected by high temperatures, so they secrete testosterone normally (thus the male secondary sex characteristics will appear normally at puberty)
(3) Diet
A balanced diet containing adequate amounts of proteins and vitamins (especially vitamins A, E, C and B ) is necessary for normal spermatogenesis.
(4) Other factors
Prolonged exposure to various types of radiations (x-ray, atomic or nuclear radiations) prolonged hypoxia certain toxins, and infections (eg mumps) all damage the seminiferous tubules and depress spermatogenesis.
Endocrinal functions of the testes
The testes secrete several male sex hormones, which are collectively called androgens, including testosterone, dihydrotestosterone, and androstenedione, Testosterone is much more abundant and potent than the other.
Epididymis
It is a highly coiled tube, that lies on the posterior border of the testis.
Parts of the epididymis
- Head attached to the upper end of the testis by 12-30 efferent ductules.
- Body.
- Tail: attached to the lower end of the testis, and continues as the vas deferens.
Sinus of epididymis: It is a recess of tunica vaginalis, which lies between the testis and the lateral side of the body of the epididymis.
How to know the side of the testis: right or left?
- Epididymis lies posterior.
- The sinus of the epididymis is directed laterally.
- Vas deferens arise from the tail of the epididymis, which is directed inferiorly.
Histological structure of the epididymis
The tubuli recti enter the mediastinum testis and form the anastomosing channels of the rete testis. Vas efferentia arise from the rete testis and unite to transport the spermatozoa into the single epididymal duct. The epididymis is surrounded by a fibrous CT capsule, tunica albuginea. In histological sections, epididymis appears as multiple oval cut sections with sperms in their lumina. The epididymal duct is lined by pseudostratified columnar epithelium formed of 2 types of cells.
- Principal cells: tall columnar with stereocilia and oval basal nuclei. They are secretory/ absorptive cells with a very large supranuclear Golgi complex.
- Basal cells: short triangular with rounded nuclei. They are the stem cells from which the columnar cells are renewed.
The epithelium is supported by vascular connective tissue, the lamina propria, and is surrounded by a few layers of smooth muscle fibers which increase towards the tail region.
Functions of the epididymis
1. Storage of sperms: where absorption of excess fluid and removal of residual bodies, not removed earlier by Sertoli cells, occur. Epididymal sperms are expelled during ejaculation.
2. Maturation of sperms in epididymis:
- Sperms removed from the seminiferous tubules are completely non-motile, and they cannot fertilize an ovum. In the epididymis, sperms develop the capability of motility by a special nutrient fluid (secreted from Sertoli cells and epididymal principal cells), even though several inhibitory proteins in the epididymal fluid still prevent final motility until after ejaculation.
- Secretion of glycolipid decapacitation factors that block the acrosomal reaction until the capacitation process occurs in the female reproductive tract just before fertilization. ”The acrosomal reaction in which the acrosomal membrane fuses with the sperm membrane creating pores through which hydrolytic and proteolytic enzymes can escape from the acrosome and penetrate the protective coverings of the ovum”.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Organs of male genital system, Structure of the testis, Functions of Sertoli cells & Leydig cells
Vas deferens function, histology, anatomy, Varicocele & Functions of Seminal vesicle
Prostate function, structure, lobes, Benign enlargement of prostate & malignant prostatic tumor
Testosterone effects, low testosterone symptoms, Hypogonadism & Hypergonadism in male