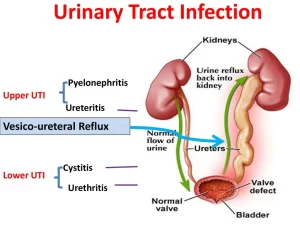
Urinary tract infections causes, types, risk factors, Upper UTI (pyelonephritis), Lower UTI (cystitis and urethritis)
A urinary tract infection (UTI) happens when bacteria, often from the skin or rectum, enter the urethra and infect the urinary tract, The infections can affect many parts of the urinary tract, but the most common type is the bladder infection (cystitis), Kidney infection (pyelonephritis) is another type of UTI, They’re less common but more serious than the bladder infections.
Urinary tract infections (UTI)
Urinary tract infection implies infection of the lower urinary tract (urinary bladder and urethra) or upper urinary tract (kidney and renal pelvis) or both.
Types of Urinary tract infection
- Lower UTI (cystitis and urethritis).
- Upper UTI (pyelonephritis).
Risk factors
- In males, this may occur during urethral instrumentation, catheterization, and cystoscopy.
- In females, short urethra, and repeated urethral trauma during intercourse facilitate entrance of bacteria to the bladder.
- Urinary outflow obstruction or bladder dysfunction, In the presence of stasis, bacteria introduced into the bladder can multiply disturbed without being flushed out or destroyed by the antimicrobial properties of the bladder mucosa.
- Diabetes mellitus. Neurogenic bladder dysfunction which predisposes to urine stasis, lowered body resistance, and increased susceptibility to infection.
- Immunosuppression and immunodeficiency.
Sources of infections
- Ascending infection; starts from the lower urinary tract (urethra and urinary bladder) and then ascends to the kidney.
- Hematogenous infection; which usually starts from the upper urinary tract kidney) then descends to the lower urinary tract.
Ascending infection
It’s the most common source of infection.
Etiology: The principal causative organisms are enteric gram-negative bacilli; E.coli is the most common one, Other important organisms are species Proteus, klebsiella, Enterobacter, and Pseudomonas.
Pathogenesis
Starts with a lower urinary tract infection. Then infection ascends from the bladder to the ureter through the incompetence of the vesicoureteral orifice (vesico ureteric reflux) which is mandatory. (This incompetence is either congenital or secondary to a persistent increase in intravesical pressure) then infected urine propel to the renal pelvis and further to renal parenchyma through open ducts at the tips of the papillae (intrarenal reflux).
Hematogenous infection
It is less common than ascending infection. It occurs by the seeding of bacteria during septicaemia and infective bacterial endocarditis. The condition is facilitated by ureteral obstruction and the use of immunosuppressive drugs. The organisms are mainly staphylococci, e.coli. It is the way through which bilharziasis induce cystitis.
Lower urinary tract infections
It leads to inflammation of the urethra (urethritis) and urinary bladder (cystitis).
Clinical picture
- All forms of cystitis are clinically characterized by a triad of symptoms: Dysuria (painful or burning micturition), Frequency (repeated micturition), and Supra-pubic pain.
- Systemic manifestations of bacteremia such as fever, chills, and malaise.
- Hematuria.
Types of cystitis
- Acute cystitis.
- Chronic cystitis.
- Chronic non-specific cystitis: is due to the persistence of infection or as sequele of acute infection.
- Chronic specific cystitis includes Bilharzial cystitis, and Tuberculous cystitis that results from descending infection from tuberculosis of the kidney and is characterized by caseating granulomatous reaction fibrosis.
Bilharzial cystitis
Grossly: Early the mucosa is congested, then displays sandy patches, multiple polypi (simple or branched), nodules, and superficial ulcers (moth-eaten appearance). Late stages lead to contracted calcified bladder which may be associated with strictures at the ureteric orifices.
Microscopically
Is characterized by the deposition of bilharzial ova within the lamina propria and extending to the muscle layer; surrounded by the localized or diffuse granulomatous reaction. The urothelium may show reactive hyperplasia with the formation of Von Brunn’s nests, Cystitis cystica, Cystitis glandularis, and in some cases there is squamous metaplasia (precancerous lesion)
Upper urinary tract infection (Pyelonephritis)
Definition: inflammation of renal parenchyma and renal pelvis.
Types
1. Acute pyelonephritis
It is an acute suppurative inflammation of renal parenchyma and renal pelvis characterized by abscess formation. It is caused by bacterial infection. (E.coli is the most common).
Morphology
Grossly: One or both kidneys may be affected. The size is normal or slightly enlarged, There are discrete yellowish raised abscesses on the external renal surface. They are haphazardly arranged, or they might be present on the upper and lower poles, or may form a single large area of suppuration. The renal pelvis and calyces are hyperemic with hemorrhagic and suppurative foci. healing occurs by fibrosis (pyelonephritis scar).
Microscopically
The characteristic histologic feature is abscess formation within the renal parenchyma, Intratubular neutrophils frequently extend into the collecting ducts, giving rise to characteristic white blood cell casts in the urine. typically. The glomeruli are NOT affected.
Clinical features
It manifests itself by:
- Sudden onset of pain at the costo-vertebral angle, fever, chills, and malaise.
- Pyuria: urine contains casts of pus.
- In Bacteriuria, urine contains casts of bacteria.
- Manifestations of LUI (dysuria, frequency, and urgency).
Fate and complications
With appropriate treatment, the disease follows a benign course with healing by fibrosis that leads to depressions in the kidney surface, associated with deformities in the pelvicalyceal system. In diabetics and those with urinary tract obstructions, the following complications may develop:
- Chronic pyelonephritis due to recurrent infection.
- Papillary necrosis (necrotizing papillitis): a rare form of pyelonephritis associated with poor prognosis. Predisposing conditions: diabetes, urinary tract obstruction, and sickle cell anemia. this lesion is marked by ischemic and suppurative necrosis of the renal papillae.
- Pyonephrosis: pyelonephritis is associated with complete obstruction of the ureter leading to accumulation of pus in the renal pelvis, calyces, and interstitial tissue; the kidney will be transformed into a bag full of pus.
- Perinephric abscess: due to rupture of the capsule and extension of the suppurative inflammation into the perinephric tissue.
2. Chronic Pyelonephritis
Chronic Pyelonephritis is a disorder in which tubulointerstitial inflammation and scarring of the renal parenchyma are associated with grossly visible scarring and deformity of the pelvicalyceal system, It is essentially the result of repeated attacks of inflammation and healing and consequently, it is an important cause of end-stage renal failure.
Types
A. Chronic non-specific pyelonephritis which is either:
- Secondary to obstruction (chronic obstructive pyelonephritis), Obstruction predisposes the kidney to infection.
- secondary to urine reflux (chronic reflux-associated pyelonephritis), It is the most common cause of chronic pyelonephritis, It results from the superimposition of a UTI on congenital vesicoureteral reflux and intrarenal reflux.
(Recurrent infections superimposed on VUR or obstruction lead to recurrent bouts of renal inflammation and scarring, which eventually causes chronic pyelonephritis).
B. Chronic specific pyelonephritis as in renal tuberculosis.
Chronic non-specific pyelonephritis
Morphology
Grossly: One or both kidneys may be involved, The hallmark is large discrete cortico-medullary scars associated with underlying calyceal blunting and deformities, The scars are usually located at the upper or lower poles of the kidney, If the lesion is bilateral, scarring is asymmetrical (D.D. with bilateral symmetrically contracted kidneys e.g. benign nephrosclerosis and chronic GN), In the obstructive type, the pelvicalyceal system is inflamed and distended, In non-obstructive type; the pelvicalyceal system is not distended.
Microscopically
The microscopic changes are largely nonspecific, and similar alterations may be seen with other chronic tubulointerstitial disorders as analgesic nephropathy.
- Chronic inflammatory cell infiltration and uneven fibrosis involving the pelvicalyceal system and parenchyma.
- Tubular atrophy and thyroidization (colloid cysts).
- Arteriolosclerosis may be caused by associated hypertension.
- Glomerulosclerosis (secondary to nephron loss).
Clinical features
It might be silent or might present with symptoms of acute pyelonephritis.
- Secondary hypertension.
- Bilateral progressive cases lead to chronic renal failure.
Chronic specific pyelonephritis (Renal tuberculosis)
Routes of infection
- Hematogenous spread of the infection from another site, most often from the lungs.
- Less commonly, it may result from ascending infection.
The renal lesions in TB may be in the form of:
- Miliary tuberculosis.
- Tuberculous pyelonephritis
Morphology:
Gross:
1. Tuberculous pyelonephritis:
- Often bilateral.
- Usually involving the medulla with replacement of the papillae by caseous tissue.
2. Miliary tuberculosis. Appears as numerous small tubercles, 1-2 mm in diameter, slightly raised above the surface, and more marked in the cortex.
Histologically: Typical granulomatous reaction.
Clinical features
- Hematuria.
- Dysuria, frequency urgency & nocturia due to bladder and urethral irritation.
- Chronic renal failure if bilateral.
Complications
Tuberculous pyonephrosis due to obstruction, Thinned-out renal parenchyma surrounds the dilated pelvis and calyces filled with caseous material.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Urinary bladder structure, function, Control of micturition by Brain & Voluntary micturition
Urinary passages function, structure of Ureter, Urinary bladder & Uvulae vesicae
Control of water balance in your body, Regulation of volume & osmolality of Body fluids
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption & secretion
Histological structure of kidneys, Uriniferous tubules & Types of nephrons
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism
Physical properties of urine, Tests to evaluate kidney function & Normal constituents of urine
Packaging of DNA, Genome, chromosomal proteins, DNA in Prokaryotes & Eukaryotes