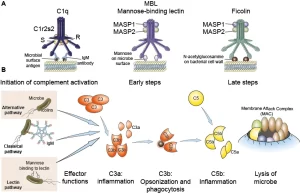
Complement system function, Importance of MHC, Classical, Lectin, and alternative Pathways
The complement system is a complex group of serum proteins, present in low concentration in normal serum, that interact with each other in a cascading fashion to protect against infectious agents. Membrane-bound proteins are also included in the complement system.
Synthesis of the complement system
Complement components are synthesized in the body by several cells: hepatic parenchymal cells, monocytes, macrophages, and intestinal epithelium.
Nomenclature of complement proteins
The complement components are designated by the letter “C” followed by a number, which is related to the order of its discovery e.g. C1. C2, C3 … etc. On cleavage of a complement component, the large fragment is given the suffix “b” e. g. C5b and the smaller fragment is given the suffix “a” e.g. C5a. Components of the alternative pathway are designated with a capital letter e.g. factor B. factor D etc…
Pathways of Complement Activation
The activation of complement components takes place in a sequential fashion, each component activating its successor protein in the cascade, Many components are pro-enzymes that must be cleaved to form active enzymes, There are three complement pathways: classical, alternative, and lectin.
Complement pathways lead to the formation of a complex enzyme (C3 convertase) capable of binding and cleaving a key protein C3, common to pathways. C3 activation is the common central event. After that, the three pathways proceed in the same fashion together through the binding of the late-acting components to form a membrane-attack complex (MAC) which is C5b6789 which becomes inserted in the lipid bilayers of foreign membranes, ultimately causing cell lysis.
The classical pathway is typically initiated by Ag-Ab complexes, in solution or on the surface of a cell thus it is triggered after the generation of specific Ab to a particular Ag. On the other hand, the activation of the alternative pathway occurs by the microbial surfaces and it can proceed in the absence of Ab.
and thus helps in the first line of defense against micro-organisms (innate immunity) and mediates an inflammatory response. Likewise, the lectin pathway bypasses antibodies and uses a lectin, mannose-binding lectin (MBL) o initiate events.
Biologic Functions of the Complement System
1 Cell Jysis: Insertion of the membrane attack complex (C5b6789) into the cell membrane leads to the lysis of many types of cells, including bacteria, tumour cells, erythrocytes, protozoa, and enveloped viruses
2 Opsonization: Cells, antigen-antibody complexes, and other particles are phagocytosed much more efficiently in the presence of C3b bound on their surfaces, because of the presence of C3b receptors on the surface of many phagocytes e.g. monocytes, macrophages, neutrophils…. etc.
3 Inflammatory function: ie. the generation of peptide fragments that regulate the features of the inflammatory and immune response:
- Chemotaxis: C5a attracts phagocytic cells, mainly polymorphs to the site of inflammation and increases their activity.
- Anaphylatoxins: C3a and C5a can produce degranulation of mast cells with the release of histamine, serotonin and other mediators which cause increased vascular permeability and smooth muscle contraction.
Regulation of the Complement System
In order to avoid constant complement activation, a regulatory network exists to terminate complement activity Several serum proteins regulate the complement system at different stages.
Major Histocompatibility complex (MHC)
Transplantation is the practice of grafting tissues or organs from one person to another or from one place to another in the same person. The main problem in transplantation between genetically non-identical persons is graft rejection, This is due to the presence of tissue antigens that differ from one individual to another and stimulate the immune response which causes the rejection.
These tissue antigens are called Human Leucocytic Antigens (HLA) or Major Histocompatibility Complex (MHC) or Transplantation antigens, There are three major histocompatibility antigens: class I, class II, & class III MHC antigens, These antigens are genetically determined by a set of genes called the major histocompatibility gene complex, which lies on a portion of the short arm of human chromosome 6, These genes occupy four regions (A,B,C and D).
Regions B, C and A determine the antigenic specificities of class I MHC surface molecules, Region D determines the antigenic specificities of class II MHC surface molecules. The region between D and B codes for certain complement components (C2, C4, factor B), and is not concerned with graft rejection. It is called class III MHC.
Class I MHC-antigens: are glycoproteins and include HLA-A, HLA-B, and HLA-C. They are found on all nucleated cells. Class I MHC enables cytotoxic T cells (Tc) to recognize foreign antigen on the surface of graft cells, tumour cells or virus infected cells and kill these cells. In other words, Tc cells (CDB) are triggered only when they recognize both antigen and class I MHC molecules in close association on the surface of target cells. This is known as MHC restriction.
Class II MHC-antigens: or HLA-D antigens are glycoproteins, and include HLA- DP, HLA- DQ and HLA-DR. These are found chiefly on antigen presenting cells (APCS) such as monocytes, macrophages, dendritic cells in lymph nodes, Langerhans cells in skin and B lymphocytes.
Helper T cells (Th) (CD4) will recognize foreign antigen on the surface of APC only if they are associated with class II MHC molecules (MHC restriction). The HLA system is extremely polymorphic, having multiple alternative forms or alleles of the gene at each known locus e.g. HLA A1, A2, A3….. etc. Both classes could be typed by: Flow cytometry or molecular techniques such as PCR.
Importance of MHC
1. Organ transplantation and graft rejection.
2. MHC restriction:
- Tc cells recognize the Ag in association with MHC I.
- Th cells recognize the Ag in association with MHC II.
3. Disease association. It is found that the presence of certain HLA antigens is often associated with a particular disease::
- HLA-B27 with ankylosing spondylitis.
- B8 with myasthenia gravis.
- DR2 with multiple sclerosis.
- DR4 with rheumatoid arthritis.
4. Paternity testing and forensic investigations (An individual inherits one maternal and one paternal chromosome 6).
You can follow science online on Youtube from this link: Science online
You can download Science online application on google Play from this link: Science online Apps on Google Play
Immunogens, antigens, antibodies, Immunoglobulin Classes & Protective Functions of Antibodies
Features and classification of viruses, Defective viruses & Viral vectors used for gene therapy
Classification of medically important Gram-negative bacilli
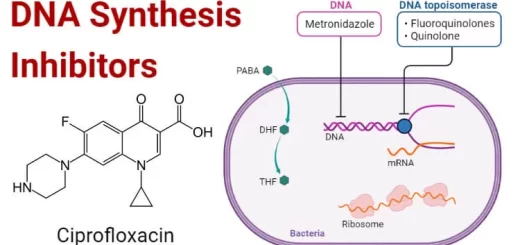
Antibiotics advantages, disadvantages, resistance & uses
Control of Drug Resistance & Bacterial resistance to chemotherapeutic agents
Staphylococci definition, diagnosis of staphylococcal infections & treatment