Types of Nucleic acid synthesis inhibitors, Bacterial metabolism inhibitors and Cell membrane inhibitors
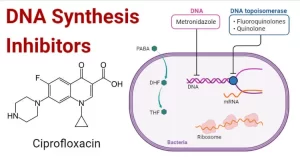
Nucleic acid inhibitor is a type of antibacterial, It acts by inhibiting the production of nucleic acids, There are two major classes of nucleic acid inhibitors: DNA inhibitors and RNA inhibitors, RNA inhibitors such as rifampin, act upon DNA-dependent RNA polymerase, DNA inhibitors such as quinolones act upon DNA gyrase as a topoisomerase inhibitor.
Nucleic acid inhibitors
Another group of DNA inhibitors, including nitrofurantoin and metronidazole, act upon anaerobic bacteria, These act by generating metabolites that are incorporated into DNA strands, which are more prone to breakage, These drugs are selectively toxic to anaerobic organisms but can affect human cells.
Nucleic acid synthesis inhibitors
Nucleic acid synthesis inhibitors are classified into:
- DNA inhibitors: quinolones and metronidazole.
- RNA inhibitors: rifampin.
Quinolones
The important quinolones are synthetic fluorinated analogs of nalidixic acid (fluoroquinolones). Fluoroquinolones are bactericidal antibiotics. They are grouped into three generations, which offer greater efficacy, a broader spectrum of antimicrobial activity, and a better safety profile than the first-generation nalidixic acid.
Pharmacokinetics
Fluoroquinolones are rapidly and almost completely absorbed after oral administration and are widely distributed in body tissues. Food ingestion does not affect the bioavailability of fluoroquinolones. Fluoroquinolones are really eliminated, therefore, their dosages should be modified in patients with moderate to severe renal insufficiency.
Classification, antimicrobial activity, and therapeutic uses of quinolones
First generation: Nalidixic acid is a non-fluorinated quinolone. It is no longer used for urinary tract infections because of the spread of E. coli quinolone-resistant strains.
Second generation: (Anti-pseudomonal fluoroquinolones): eg.ciprofloxacin, ofloxacin.
Spectrum: it is active against many Gram-negative organisms (including Pseudomonas) with limited activity against some Gram-positive organisms.
Therapeutic Uses:
- Complicated urinary tract infections.
- Gastrointestinal infections caused by Salmonella, Shigella, and Campylobacter.
- Hospital-acquired pneumonia.
It is not recommended as an empiric first-line drug in uncomplicated urinary tract infections
Third generation: (Respiratory fluoroquinolones): eg. levofloxacin.
Spectrum: It is active against Gram-negative (but less active against Pseudomonas), with improved activity against Gram-positive cocci (Streptococcus pneumoniae) and atypical organisms.
Therapeutic Uses
- Complicated urinary tract infections.
- Acute otitis media and sinusitis.
- Community-and hospital-acquired pneumonia.
Fourth generation: eg. moxifloxacin.
Spectrum: It is active against Gram-negative organisms (but less active against Pseudomonas), with enhanced activity against Gram-positive cocci and anaerobes.
Therapeutic Uses
- Community and hospital-acquired pneumonia.
- Intra-abdominal infections.
Adverse Reactions
- Gastrointestinal upsets.
- Skin rash and photosensitivity.
- CNS reactions to insomnia and increased incidence of seizures in epileptic patients.
- Abnormal liver function tests and hypo or hyperglycemia.
- Tendon damage and rupture, especially if combined with steroids.
- Inhibition of hepatic cytochrome 450 leads to drug interactions.
- Prolongation of QT intervals.
- Teratogenicity: Sometimes, they are used during pregnancy if the better-studied antibiotics are ineffective with ciprofloxacin being the preferred option. Herein, the benefit will outweigh the risk.
The use of fluoroquinolones in children: Because of arthropathy observed in juvenile animals, fluoroquinolones should not be used in pediatric patients for routine infections when other safe and effective antimicrobials are available. However, they should be considered in life-threatening and difficult-to-treat infections when alternative agents can’t be used.
Metronidazole
Spectrum:
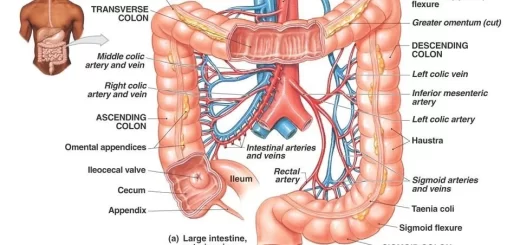
Metronidazole is effective against nearly all anaerobic Gram-negative bacteria and most anaerobic Gram-positive bacteria. It is one of the few antibiotics that have activity against Clostridium difficile and is the treatment of choice for infections caused by this organism (pseudomembranous colitis). Helicobacter pylori is also frequently susceptible. It is an antiprotozoal agent against Giardia, Trichomonas, and Entamoeba histolytica.
Adverse Reactions
- Gastrointestinal upsets are the most common.
- Metallic Taste.
- Seizures and cumulative peripheral neuropathy are rare but serious, therefore multiple therapeutic courses for recurrent C. difficile infection should be avoided.
Drug Interactions
- Since metronidazole can prolong QT intervals drugs with a possible risk for QT prolongation should be used cautiously with it. e.g., clarithromycin azithromycin.
- It is an inhibitor of cytochrome P450, thus it can potentiate the anticoagulant effect of warfarin, resulting in the prolongation of prothrombin time and increased risk of bleeding.
Tinidazole is another nitroimidazole with selective activity against anaerobic bacteria and protozoa Compared to metronidazole, it has a longer half-life and is better tolerated. Moreover, it is administered for a shorter duration, e.g., in the treatment of amebic colitis.
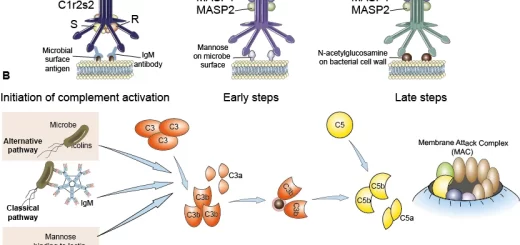
Bacterial metabolism inhibitors (Folate antagonists)
They include sulfonamides, trimethoprim, and pyrimethamine (antifolate in protozoa).
1. Sulfonamides
Spectrum: Sulfonamides have bacteriostatic activity against Gram-positive cocci and Gram-negative bacilli, however, antimicrobial resistance is increasingly becoming problematic. They also have activity against Toxoplasma and Pneumocystis jirovecii.
Pharmacokinetics
They are bound to plasma albumin. They can displace bilirubin and other drugs from their albumin-binding sites. They cross the blood-brain barrier. They can pass the placental barrier and into breast milk.
Therapeutic Uses
- A combination of sulfadiazine with pyrimethamine is used for the treatment of toxoplasmosis.
- Sulphamethoxazole (SMX) is usually used in combination with trimethoprim (TMP) as Cotrimoxazole.
- Cotrimoxazole.
It is a combination of 400 mg SMX + 80 mg TMP. It is also available as 800 mg SMX and 160 mg TMP. This combination produces synergistic antimicrobial activity.
Therapeutic Uses
- Treatment of Urinary tract infections.
- Treatment and prophylaxis of Pneumocystis pneumonia in immunocompromised patients, who have malignancy or HIV and who are taking immune-suppressive drugs.
- Treatment of Toxoplasmosis.
Adverse Reactions
1. Hematologic disturbance:
- Methemoglobinemia: Methemoglobin cannot bind oxygen, resulting in functional anemia and bluish-brown discoloration of the skin.
- The inhibition of the folate metabolism by trimethoprim can cause dose-related leukopenia and megaloblastosis.
- Acute hemolytic anemia in patients with glucose-6-phosphate dehydrogenase deficiency.
- Thrombocytopenia.
2. Hypersensitivity reactions: could be manifested as fever and skin rashes.
3. Crystalluria: sulfonamides are relatively insoluble in the acid environment and tend to precipitate in the renal tubules, Adequate hydration and alkalization decrease this adverse reaction.
4. Teratogenicity Exposure to trimethoprim-sulfamethoxazole during the first-trimester lead to an increased risk of structural malformations due to the antifolate effect of TMP, The risk of major malformations, however, is reduced with supplementation with folic acid, However, sulfamethoxazole treatment of women at a 32-week gestation period or later increases the risk of hyperbilirubinemia resulting from the drug’s displacement of bilirubin from albumin.
Drug Interactions
- Both TMP and SMX are inhibitors of two isoenzymes of the cytochrome P450 enzyme system. Consequently, drugs metabolized by the same cytochrome P450 enzymes accumulate during treatment with TMP-SMX. They could increase the risk of sulfonylureas-induced hypoglycemia and the risk of warfaring-induced bleeding.
- In children receiving methotrexate treatment with TMP-SMX decreases renal clearance of methotrexate and increases the risk of its toxicity.
Contraindications
- Infants less than 2 months, pregnancy, and during lactation.
- Patients with impaired renal functions.
- Patients with preexisting blood dyscrasias or bone suppression.
Cell membrane inhibitors
Colistin is a polymyxin antibiotic. It has activity against many Gram-negative bacteria including those resistant to other antibiotics, e.g., Carbapenem-resistant Enterobacteriaceae. Its use should be reserved for organisms resistant to other antibiotics.
Adverse Reactions: nephrotoxicity and neurotoxicity.
Specific urinary antiseptics
Specific urinary antiseptics produce their antibacterial effect only after being concentrated in the urine. They don’t achieve effective plasma concentration for the treatment of systemic infections. Specific urinary antiseptics include Fosfomycin and nitrofurantoin
1. Fosfomycin
Spectrum: Fosfomycin demonstrates excellent in-vitro activity against most common uropathogens isolates, Due to its unique structure and mechanism of action, cross-resistance with other antimicrobial agents is unlikely.
Pharmacokinetics
Fosfomycin is rapidly absorbed after oral administration and distributes well to the kidneys, bladder, and prostate. It is not metabolized but rather is excreted unchanged in the urine by glomerular filtration. An effective Fosfomycin urinary concentration against E. coli has been reported for 80 hours following oral administration; allowing for a one-time dose for the treatment of urinary tract infections. No dosage adjustments are required in elderly patients, pregnant patients, or either renal or hepatic impairment.
Therapeutic Use
Fosfomycin is recommended as a first-line antimicrobial drug for the treatment of acute complicated cystitis, It is safe in pregnancy and lactation.
2. Nitrofurantoin
Spectrum: Nitrofurantoin is active against most Gram-positive cocci and E. coli, Pseudomonas species are naturally resistant as are many Proteus species.
Therapeutic Use
Acute uncomplicated cystitis, in which 5-day therapy is recommended.
Adverse Reactions
Gastrointestinal upsets are common, and Hemolytic reactions may occur, especially in patients with glucose-6-phosphatase dehydrogenase deficiency. Acute pulmonary toxicity might occur especially in patients with pre-existing lung disease and in elderly females. The patient could present with dyspnea, fatigue, and cough, It is reversible on drug discontinuation.
Contraindications
Nitrofurantoin can be used during pregnancy, however, It is better to be avoided near term (i.e., 38-42 weeks) because of its potential to cause hemolytic anemia in the newborn, It is safe during lactation.
Drug interactions
1. Antacids containing magnesium trisilicate reduce nitrofurantoin absorption.
2. Uricosuric drugs, such as probenecid can inhibit renal tubular secretion of nitrofurantoin. The resulting increase in nitrofurantoin serum levels may increase toxicity, and its decreased urinary levels lessen urinary tract antibacterial efficacy.
You can follow science online on Youtube from this link: Science online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Types of protein synthesis inhibitors antibiotics & Uses of individual aminoglycosides
Antibacterial drugs definition, use & types, Penicillin classification & Importance
Antimicrobial drugs types, use, side effects, resistance & Empiric antimicrobial therapy
Vaccines types, Live vaccines, Inactivated vaccines, Subunit vaccines, Naked DNA & mRNA vaccines