Female mammary glands (breast), signs of breast cancer and Mammary gland abnormalities
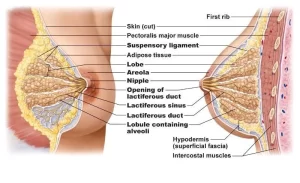
The female mammary gland (breast) is an exocrine gland that is concerned with milk production in lactating females. It is a modified apocrine sweat gland (compound tubulo-alveolar), and the glandular tissues are located in the fatty layer of the superficial fascia of the pectoral region. In male, the glandular tissue is rudimentary with scanty fat around it.
Female mammary glands (breast)
Shape: Hemispherical in shape has an extension into the axilla, called the axillary tail. Some individual variations may happen according to sex, age, body weight, and lactiferous status.
Size and contour: They are variable, but the location and size of its base are fairly constant.
Base of the mammary gland
It rests upon the deep fascia covering pectoralis major (PM) and serratus anterior (SA), and external oblique (EO) muscles. The base extends from the 2nd to the 6th ribs and from the lateral margin of the sternum to the mid-axillary line. The nipple in the male and preadolescent females lies opposite to 4th or 5th intercostal space. The breast is separated from the underlying muscles by loose areolar tissue. superficial to deep fascia, called retro-mammary space.
Arterial supply
Perforating branches of the internal thoracic artery and anterior intercostal arteries, Branches from the lateral thoracic and thoraco-acromial branches of the axillary artery.
Venous drainage
Through veins accompanying the supplying arteries.
Lymphatic drainage
1. Superficial lymphatics: to sub-areolar and circumareolar lymphatic plexus.
2. Deep lymphatics:
- Upper lateral & central parts of the breast: to apical group of axillary lymph nodes.
- Lower lateral: to the pectoral group of axillary lymph nodes.
- Upper medial: to parasternal (internal mammary) lymph nodes.
- Lower medial: to anterior abdominal wall LNS (rectus sheath and sub-peritoneal plexus).
- Tail of the axilla: to the posterior (subscapular) group of axillary lymph nodes.
Clinical notes (Applied anatomy):
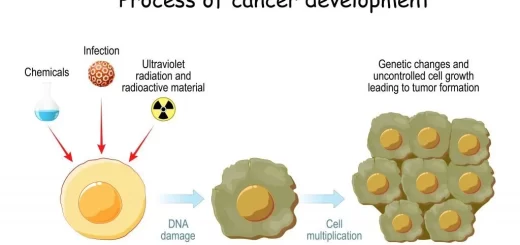
a)- Anatomical analysis of the physical signs of cancer of the breast:
- Invasion of the deep fascia (fibrosis of retro-mammary space, leads to fixation of the breast (Advanced cases).
- Invasion of ligaments leads the suspensory to shortening of the ligaments-dimpling of overlying skin.
- If tumor tissue blocks the deep lymphatics, lymph from the skin cannot be drained away, and the skin becomes pitted and oedematous, resemble the texture of the skin of an orange (Peau d’ orange).
- Invasion of the lactiferous ducts leads to shortening of the ducts ——- retracted (inverted) nipple.
b)- In case of breast abscess incision must be done in a radial direction, to minimize ducts damage.
Histological Structure of mammary gland
I- The covering skin
The mammary gland is covered by thin skin rich in subcutaneous fat. The covering skin forms a cylindrical, brownish elevation, and the nipple that consists of dense connective tissue and smooth muscle fibers. The nipple has 15-20 pore-like openings; each is belonging to one lactiferous duct, the excretory ducts of the mammary gland.
The lactiferous ducts become dilated shortly before their terminal opening at the summit of the nipple to form the lactiferous sinuses. The pinkish-colored area around the nipple is the areola. It becomes highly pigmented during pregnancy.
The skin covering the nipple and areola is richly supplied by free nerve endings. Meissner’s and Pacinian corpuscles. This sensory innervation of the nipple and areola is important because their stimulation, by the suckling infant, initiates and maintains the secretion of milk.
Il- Mammary gland in different physiological periods and its hormonal control
The glandular tissue is formed of connective tissue stroma and secretory parenchyma. During childhood, the mammary glands are rudimentary, consisting only of a few ducts lined with flat epithelial cells, which are surrounded by a small amount of connective tissue (stroma).
A. Resting mammary gland (in adult non-pregnant female)
At puberty, the mammary glands develop mainly by the effects of estrogens and progesterone secreted from the ovaries. Other hormones such as thyroid hormone, adrenal corticosteroids and insulin have only a permissive effect on the development of breasts.
Role of estrogens: estrogens cause the proliferation of the ducts, deposition of fat, growth of stroma and development of nipples. Such effects require the actions of other hormones, particularly the growth hormone which causes protein deposition in the glandular cells which is essential to glandular growth.
Role of progesterone: It causes growth of the lobules and alveoli of the breast.
Histologically:
Stroma
The mammary gland has no capsule. Thick interlobar connective tissue septa arise from the reticular layer of the dermis. radiating from the nipple and extend to divide the gland into 15-20 irregular lobes. Each lobe is further subdivided into lobules by interlobular septa formed of connective tissue rich in adipose tissue.
Highly cellular intralobular connective tissue containing fibroblasts, lymphocytes, plasma cells and macrophages that surrounds the duct system. This connective tissue arises from the papillary layer of the dermis.
Parenchyma
Each lobule is formed of several small, branching intralobular ducts, however, the secretory units (the alveoli) are small and rudimentary. The intralobular ducts, lined by cuboidal or low columnar cells are present either singly or in groups surrounded by cellular intralobular connective tissue.
In larger interlobular ducts the epithelium changes from columnar to two layers of cuboidal cells. These ducts unite into a single lactiferous duct that opens separately on the summit of the nipple Myoepithelial cells are present between the epithelium of the ducts and their basal lamina.
The lactiferous duct and its dilated lactiferous sinus are lined by stratified squamous epithelium. During each menstrual cycle, especially at the time of ovulation, some histological changes occur in the mammary glands in the form of proliferation of the duct system and increased vascularity of the intralobular connective tissue.
B. Mammary gland during pregnancy
Full development of the breasts occurs by the effects of high levels of estrogens and progesterone as well as by prolactin and human chorionic somatomammotropin
Stroma & parenchyma
The glands undergo massive growth as a result of proliferation and branching of the duct system. The secretory alveoli proliferate by budding from the ends of the intralobular ducts. Late in pregnancy, well-established lobules that contain secretory alveoli, in addition to intralobular ducts can be recognized.
The glandular alveoli begin to secrete the colostrum, a serous fluid rich in protein and with low-fat content. Such secretory activity causes further enlargement of the breasts. Active milk production is not established until a few days after delivery.
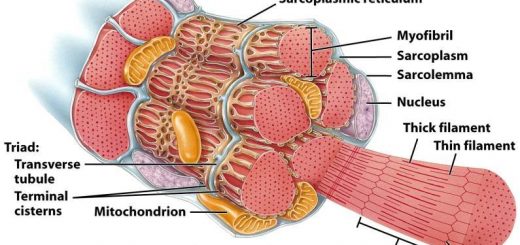
C. Lactating mammary gland
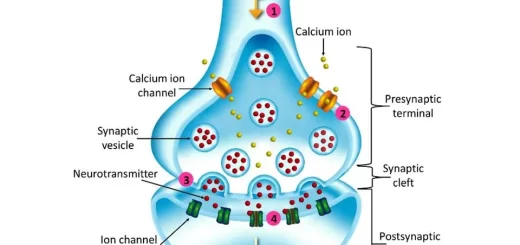
After delivery, the alveoli of the mammary gland start active milk production andlactation. Milk synthesis is an active secretory process, which is stimulated by prolactin hormone and chorionic somatomammotropin whereas milk ejection is caused by oxytocin.
Stroma & parenchyma
The lobular pattern of the gland is very evident, comprising 15-20 irregular lobes distended with a large number of secretory alveoli with little intralobular connective tissue. The connective tissue stroma and the adipose tissue decrease. The interlobar and interlobular connective tissue become reduced to thin septa.
Milk is produced inside the columnar epithelial cells of the secretory alveoli and accumulates in their lumina and inside the ducts. Milk secretion involves the following mechanisms:
- Merocrine secretion of milk protein, packaged in secretory granules and exocytosed at the apical end of the cell.
- Apocrine secretion of relatively large lipid droplets, extruded from the cell along with a small amount of cytoplasm and surrounded by a portion of the apical cell membrane.
The alveoli are surrounded by stellate myoepithelial cells, their processes surround and pass in between the secretory cells of the alveoli to squeeze them and push the milk through their lumina to the duct system. Spindle-shaped myoepithelial cells are oriented longitudinally along the smallest ducts between the epithelium and the basal lamina. The act of suckling initiates hormone production and establishes milk secretion, thus the alveoli of adjacent lobules may appear in different grades of activity:
- Groups of alveoli consist of high pyramidal cells with milk granules at the apical parts of the cells,
- Others show milk accumulated in the ducts and lumina of the alveoli with the apical parts of the cells are shed with milk leaving nearly cuboidal cells.
- Alveoli, from which the milk was suckled, show cuboidal cells with empty lumina,
- Some other alveoli show regenerating columnar cells but still without milk granules in their apical parts.
D. Mammary gland of menopause
After menopause, involution of the glands occurs, characterized by:
- Reduction in size and atrophy of its secretory portion and part of the excretory ducts.
- Striking atrophic changes occur in the connective tissue stroma with loss of collagen and elastic fibers.
Development of the mammary gland
The first indication of mammary glands is found in the form of a band-like thickening of the epidermis, the mammary line or mammary ridge, In a 7-week embryo, this line extends on each side of the body from the base of the forelimb to the region of the hindlimb.
In animals, several mammary glands are formed along this ridge, In human, the ridge disappears except for a small part in the pectoral region, This localized area thickens, becomes slightly depressed, and sends off 15 to 20 solid cords, which in turn give rise to small, solid buds, They grow into the underlying mesenchyme.
By the end of prenatal life, the epithelial cords are canalized and form the lactiferous ducts, and the buds form small ducts and alveoli of the gland, Initially, the lactiferous ducts open into a small epithelial pit, This pit is transformed into the nipple by the proliferation of the underlying mesenchyme, At the fifth month, the areola is recognized as a circular pigmented area of skin around the future nipple
Mammary gland abnormalities
- Polythelia Supernumerary nipples occasionally occur along with a line corresponding to the position of the milk ridge, They are liable to be mistaken for moles.
- Polymastia: It occurs when a remnant of the mammary line develops into a complete breast.
- Retracted nipple or inverted nipple: The retracted nipple is a failure in the development of the nipple during its later stages, It is important clinically because normal suckling of an infant cannot take place, and the nipple is prone to infection.
- Micromastia: An excessively small breast on one side occasionally occurs, resulting from a lack of development.
- Macromastia: Diffuse hypertrophy of one or both breasts occasionally occurs at puberty in otherwise normal girls.
- Gynecomastia: Unilateral or bilateral enlargement of the male breast occasionally occurs, usually, at puberty, The cause is unknown, but the condition is probably related to some form of hormonal imbalance.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Female reproductive system organs, functions, anatomy and Histological structure of the uterus
Fallopian tubes function, location, anatomy and Histological structure of vagina
Monthly ovarian cycle, Corpus luteum & menstrual cycle phases, function and hormones
Indifferent gonads, Development of gonads and genital ducts, Abnormalities of testis and ovary