Hepatic Tumors, Benign tumors, Hepatocellular tumors, Mesenchymal tumors, Biliary & cystic lesions
Hepatic tumors are also called Liver tumors, they are abnormal growth of liver cells on or in the liver, Hepatic tumors are classified as benign (non-cancerous) or malignant (cancerous) growths, They may be discovered on medical imaging, and the diagnosis is often confirmed with liver biopsy, Symptoms of liver masses vary from being asymptomatic to patients presenting with an abdominal mass, hepatomegaly, abdominal pain, jaundice, or some other liver dysfunction.
Hepatic Tumors
The liver breaks down and stores nutrients absorbed from the intestine, it makes clotting factors to protect you from bleeding too, and breaks down alcohol, drugs, and toxic wastes in the blood. Liver tumors are growths on or in the liver. hepatic tumors that are malignant – growing into nearby tissue or spreading to other parts of the body – are liver cancer, Hepatic tumors can be classified as benign or malignant.
Benign tumors
- Hepatocellular tumors.
- Biliary and cystic lesions.
- Mesenchymal tumors.
Hepatocellular tumors
Hepatocellular adenoma
- Women are affected more than men, usually within childbearing years, usually single.
- May be Asymptomatic, so most cases are discovered accidentally.
- Pressure manifestation on nearby structures such as biliary radicles and vascular structures.
- Rt. Hypochondrial pain due to space-occupying lesions that stretch on the capsule.
- Diffuse abdominal pain with intraperitoneal hemorrhage if the tumor ruptures.
- Malignant transformation in up to 8% of all patients & up to 40-50% of men.
Risk factors for hepatocellular adenomas
- Long-standing intake of OCP (up to 90% of cases had a history of long use of OCP).
- Glycogen storage diseases, which is a rare entity of genetic disease.
- Long-standing intake of anabolic steroids.
Diagnosis
Serology
The lab is normal (transaminases, alkaline phosphatase, AFP), except if there is obstructive jaundice there will be elevated serum bilirubin due to compression on bile ducts.
Imaging
- Usually, hepatic adenomas are detected by routine abdominal US (cheap & sensitive).
- Then, contrast-enhanced US dynamic MRI is needed for differentiation between adenoma & FNH.
Liver biopsy
If the nature of the tumor is not conclusive by imaging, we will proceed to a Liver biopsy.
Treatment
- Stop risk factors as: hormones, and anabolic steroids, it will help to stabilize the tumor and make it stationary.
- Some cases show regression of the tumor according to response to stop of risk and need follow-up.
- Surgical excision if Symptomatic more than 5 cm in diameter, men due to high rate of malignant transformation.
- If we face complications of tumor-like bleeding adenomas: Trans- Arterial Embolization (TAE) to occlude the bleeding vessel.
Focal Nodular Hyperplasia (FNH)
- It is the 2nd most frequent benign hepatic tumor originating from hepatocytes (after hemangioma: which is the 1st most frequent benign hepatic tumor and is one of the mesenchymal hepatic tumors originating from mesenchyme).
- FNH is not a contraindication in pregnancy or the use of OCP, unlike hemangioma in which hormonal replacement therapy or hormones, in general, induce large hemangiomas.
- Lesions are multiple in 1/3 of patients, most lesions are less than 2cm in diameter.
- FNH is thought to be a hyperplastic response to an artery-to-portal vein shunt.
Diagnosis
Imaging
- Determination of follicular lesions whether single or multiple and then confirm by contrast US and MRI.
- But if the complete diagnosis is not achieved by imaging modalities, we will proceed to biopsy.
- By classical abdominal US, we will detect only focal lesions, so we should proceed to contrast-enhanced US or MRI to know the nature of the tumor and confirm and finalize the diagnosis, and if no final diagnosis is obtained by imaging modalities, we will proceed to liver biopsy.
Liver biopsy
- Histologically: the lesion consists of normal hepatocytes with regions of fibrous tissue containing large arteries & proliferating bile ducts with a central scar in up to 60% of cases.
- The background liver is normal.
Treatment
- FNH is a STATIC lesion (stationary lesion passing through a stationary course where rupture & malignant transformation are RARE with no increase in its size.
- Thus, the role is conservative, close observation with follow-up on regular intervals except if large, symptomatic, or pedunculated, so, think about surgery.
Nodular regenerative hyperplasia (NRH)
NRH is a nonspecific response to the obliteration of small portal veins, this obliteration is usually due to:
- Systemic vasculitis (RA, PAN, SLE, SS).
- Portal vein thrombosis (hypercoagulable state).
- Neoplastic infiltration (lymphoma).
- Toxic injury by drugs (Methotrexate, Azathioprine).
All these causes are related to portal vein thrombosis and this thrombosis and obliteration induce the formation of NRH, so it is a neoplastic lesion in response to portal vein thrombosis and obliteration, NRH appears as micro-nodules (1-2 mm in diameter delineated by regions of atrophy without fibrous septa, NRH may be asymptomatic or presented with PHTN
Biliary and cystic lesions
- Bile duct adenoma.
- Biliary adenofibroma.
- Biliary Papillomatosis: Specific and unique neoplasm, Neoplasia of the biliary tree associated with thick mucus secretion that may cause biliary obstruction without obvious actual tumor mass.
- Simple hepatic cyst. Solitary non-parasitic cysts are usually developmental. Just follow-up.
- Polycystic disease: multiple cysts may involve the liver, lung, and kidney as part of systemic polycystic lung and kidney diseases.
Mesenchymal tumors
Hemangloma (Cavernous Hemangioma)
- It is the first and most common benign hepatic tumor occurring in 5-10% of the population.
- Small lesions: They are asymptomatic.
- Large or multiple lesions: May present with right hypochondrial pain, Mass effect, so it may cause pressure effects on nearby structures, Vascular bruit may be heard, Rupture is rare and malignant transformation does not occur.
- Lesions may be enlarged during pregnancy and medication with OCP, so females in the childbearing period with Hemangioma should be followed for enlargement of the tumor and development of its complications.
Peliosis Hepatis
- Blood-filled cavities BUT walls do not have well-developed structures as in hemangioma.
- The history of anabolic steroids is usually positive.
Angiomyolipoma
The rare tumor occurs in women more than men (5:1) with a mean age in the fifth decade not occurring in the childbearing period like hepatocellular adenoma, usually solitary, Lesions have mixed histological pattern lipomatous, myomatous, angiomatous, and trabecular patterns of tumor.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
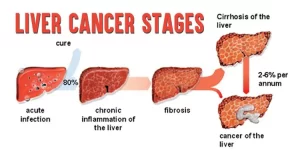
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Liver Cirrhosis causes, symptoms, treatment & stages, Liver Biopsy and treatment of PHTN
Viral hepatitis, HDV symptoms, Treatment of acute HCV, Occult hepatitis C and HEV
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Liver development, congenital anomalies, function & Pancreas development