Function of Calcium, phosphorus, Copper, Zinc and Iodine in human body
Calcium helps your body to build and maintain strong bones and carry out many important functions, It is the most abundant mineral in the body, It helps blood vessels move blood throughout your body and helps release hormones that affect many functions in your body, It plays an important role in blood clotting, helping muscles to contract, and regulating normal heart rhythms and nerve functions.
Calcium
Daily requirements:
- Infants 360-540 mg/day
- Adults 800 mg/day
- Children (1-18 years) 0.8-1.2 g/day
- During pregnancy and lactation 1.2 g/day.
Sources of calcium
Milk and cheese are the major sources, and egg yolk, vegetables, and cereals are good sources of calcium.
Absorption of calcium
Absorption of calcium occurs in the upper part of the small intestine. 1,25 dihydroxycholecalciferol which is formed by 1-hydroxylation of 25-hydroxycholecalciferol (formed in the liver) in the kidney increases active calcium absorption in the intestine by induction of formation of mRNA for the synthesis of calcium-binding proteins.
So, the active form of vitamin D3 acts as a hormone secreted in the kidney and its target organ in the intestine and there is a feedback regulation between serum calcium level and 1,25 dihydroxycholecalciferol, i.e. when there is increased serum calcium, the level of the hormone is decreased and calcium absorption is diminished.
Factors that help calcium absorption are:
- Vitamin D
- Proteins such as calcium are more soluble in amino acids than in water;
- Acidity, the low pH helps calcium absorption;
- Lactose of milk helps calcium absorption as it is changed in the intestine into lactic acid which lowers the pH.
Factors that inhibit calcium absorption are:
- Excess phosphorus inhibits calcium absorption as it forms insoluble calcium phosphate salts A ratio of Ca P between 1: 2 to 2: 1 is the most ideal for the absorption of both calcium and phosphorus.
- Excess oxalates in the diet precipitate calcium.
- Excess phytates form calcium salt (phytin).
- Excess fats as in cases of impaired fat absorption, inhibit calcium absorption as calcium salts of fatty acids (soap) which are insoluble are formed.
Distribution of calcium
The total body content of calcium is about 1-1.2 Kg. 99% of total body calcium is present in the skeleton as crystalline calcium phosphate in the hydroxyapatite (Ca10 [PO4]6[OH]2). 1% of total body calcium is present in body fluids, where it is, in part ionized and this ionized fraction is an important part for the physiologic activity of calcium
Plasma level
Varies between 9-11 mg/dL. The plasma calcium exists in three fractions:
- lonized (diffusible) calcium (53%).
- Protein-bound (non-diffusible) calcium.
- Complexed citrate (diffusible).
Calcium metabolism
The regulation of calcium metabolism depends on
- Vitamin D: explained under absorption.
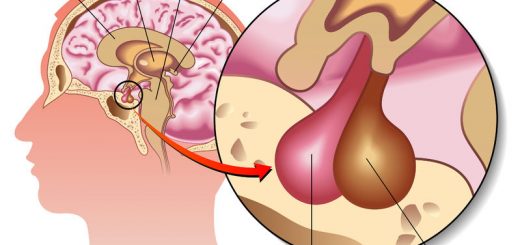
- The parathyroid hormone leads to: (a) Increased serum calcium and lowered serum phosphorus; (b) Increased urinary excretion of phosphorus and decreased urinary excretion of calcium; (c) Mobilization of calcium from the bones; (d) activation of vitamin D to 1,25-dihydroxycholecalciferol.
- Calcitonin hormone (Ca lowering hormone) through: (a) Effect on bones opposite to parathormone; (b) increased calcium excretion by the kidney, and (c) inhibition of 1,25 dihydroxycholecalciferol synthesis.
The calcium/phosphorus ratio in the serum is important for normal ossification. The product of CaxP in normal adults is about 50, and in infants, it may reach up to 70. In rickets, this product may be below 30. Ca x P product is the result of the multiplication of serum Ca level in mg/dl. by serum phosphorus level in mg/dL.
Functions of calcium
It is important for:
- It is important for the calcification of bones and teeth.
- Blood clotting as an activator of thrombokinase.
- It is important for normal contractility and excitability of heart muscles and nerves;
- It decreases cell membrane permeability and so it is used in the treatment of allergic conditions.
Abnormal levels of calcium
The increased or decreased serum calcium level may be due to diseases of the parathyroid, kidney or disturbed vitamin D level.
1. Diseases of the parathyroids
- In hyperparathyroidism: There is hypercalcemia hypophosphatemia, hyperphosphaturia and mobilization of calcium from the bones.
- In hypoparathyroidism, The serum calcium level is below 7 mg/dl. hyperphosphatemia and hypophosphaturia. Hypocalcemia leads to tetany.
2. Osteoporosis
Results with low calcium and high protein intake and it is common in females after menopause.
3. Rickets
Faulty calcification of bones in infants due to low vitamin D content of the body. There is low serum and urinary calcium and phosphorus level. The Ca x P product is below 30.
Phosphorus
Daily requirements: Since calcium is usually related to phosphorus in foods, the same daily allowances for calcium are required for phosphorus in adults. In infants, a ratio of 1.5 to 1 of calcium to phosphorus in the diet is required.
Sources of phosphorus
Milk and milk products, proteins such as fish products.
Distribution of phosphorus
The normal human body contains 0.7 to 0.9 Kg phosphorus, 80% is present with calcium in bones and teeth, 10% is present in combination with proteins, lipids, and carbohydrates in blood and muscles, and 10% in various chemical compounds as coenzymes, DNA and RNA and creatine phosphate.
Plasma level
Adults 3-4.5 mg/dL, children up to 7 mg/dL.
Metabolism of phosphorus
The metabolism of phosphorus is closely related to that of calcium and to summarize:
- Parathyroid hormone lowers serum phosphorus and increases its urinary excretion;
- Vitamin D helps intestinal absorption of phosphorus;
- Increased carbohydrate metabolism (after meals) is accompanied by a temporary decrease in serum phosphorus;
- in diabetes mellitus, there is a lower concentration of organic phosphorus and higher serum inorganic phosphorus:
- Growth hormone increases serum phosphorus level.
Functions of phosphorus
- Enters the formation of bones and teeth.
- Formation of high-energy compounds such as ATP and creatine phosphate.
- Enters the formation of coenzymes such as NAD, NADP, and FAD
- Enters in the metabolism of carbohydrates as esters of hexoses, pentoses, and trioses
- It is important in the metabolism of lipids for the biosynthesis of phospholipids present in cell membranes.
- It enters the structure of nucleotides and nucleic acids.
- It is important for blood buffers as salts of NaH2PO4 and Na2HPO4.
Abnormal levels of phosphorus
- Hypophosphatemia: With hypophosphaturia as in rickets.
- Hyperphosphatemia: As in renal failure, hypoparathyroidism and acromegaly.
Trace elements
Essential trace elements, A trace element to be essential, it must fulfill the following criteria.
- It must be present in healthy tissues.
- Its concentration from person to person is almost constant.
- Its deficiency produces certain clinical manifestations.
- its addition to diet must prevent these deficiency manifestations.
- It has a certain biochemical role.
The essential trace elements are iron, copper, zinc. iodine, manganese, cobalt, molybdenum, selenium, chromium, and fluorine.
Copper
Sources: Shellfish and liver are the main sources of copper in the diet
Distribution of copper
The total body content of copper in adults is about 100-150 mg present mainly in the liver, muscles, and bones. The copper-containing compounds in the body are:
- Cytochrome C oxidase.
- Superoxide dismutase which is given different names (e.g erythrocuprein in RBCs, hepatocuprein in the liver and cerebrocuprein in the brain).
- Enzymes such as tyrosinase, amine oxidase, and DOPA hydroxylase.
- Ceruloplasmin, the copper-binding protein in the plasma (30 mg/dL) and it is also called ferroxidase.
Plasma copper level
Plasma copper level varies between 50 and 150 μg/dl with an average of 90 μg/dl. Plasma copper is present in two forms:
- 80-90% tightly bound to protein ceruloplasmin.
- 10-20% loosely bound to serum albumin.
Functions of copper
- Copper is present in some metalloenzymes, e.g. cytochrome C oxidase, superoxide dismutase (cytosolic), amine oxidase, tyrosinase and dopamine hydroxylase.
- Copper is important for hemoglobin biosynthesis as it is important for iron metabolism.
- Copper is important for pigment formation, e.g. melanin.
- Copper is important for normal bone formation.
Copper deficiency
This is a very rare condition, characterised by hypochromic anaemia, bone disorders (thin cortices and fractures) and discolored hair.
Wilson’s disease (Hepatolenticular degeneration)
This is an inborn error of metabolism inherited as the autosomal recessive character. The disease is characterised by excessive accumulation of copper in the liver and brain, as well as excessive urinary copper excretion. There is a low serum copper level. The condition is due to the defective formation of ceruloplasmin which is important for the mobilization of copper from the tissues.
Zinc
- Daily requirements: Normal man requires about 5-15 mg/day.
- Sources: Meat, liver, eggs, and fish are major sources of zinc in the diet.
- Plasma level: The plasma level of zinc varies from 50 to 150 μg/dL.
- Distribution: The total body content of zinc in adults varies between 1.4 to 2.3 g. 20% of this amount is present in the skin, and the remaining amount is present in the pancreas, bones, teeth, prostate, and choroid of the eye.
- Deficiency: Zinc deficiency in man leads to an impaired taste sensation, poor appetite, retarded growth, hypogonadism, and impaired wound healing.
Functions of Zinc
Zinc is important for:
- Normal growth, reproduction, and wound healing.
- Storage and release of insulin.
- The function of some enzymes, eg alkaline phosphatase, and carbonic anhydrase, thymidine kinase, carboxypeptidase, and retinine reductase.
Iodine
- Sources: Sea foods are rich sources of iodine.
- Function: lodine is important for the biosynthesis of thyroid hormones.
- Deficiency: lodine deficiency may lead to Goiter, especially in the desert and high mountains.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Vitamins types & function, Sources of vitamin A & Deficiency of vitamin E
Water soluble vitamins, Vitamin B complex benefits, side effects, sources & deficiency
Benefits of taking Vitamin B complex & vitamin C, sources of Vitamin B6, Biotin & Lipoic Acid
Mineral metabolism, types, disorders, function of Sodium and Potassium