Anomalies of the bladder and urethra, Urinary tract abnormalities symptoms
Anomalies of the bladder and urethra are developmental issues that occur during fetal formation. They can affect the structure, function, or both of these urinary organs. Diagnosis of bladder and urethral anomalies often involves prenatal ultrasounds, followed by postnatal imaging tests like X-rays, ultrasounds, or cystography (special X-ray with contrast dye) after birth.
Anomalies of the bladder and urethra
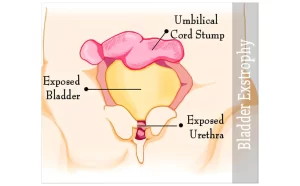
1. Ectopia Vesicae (Bladder Exstrophy)
Definition:
- Congenital absence of the anterior abdominal wall below the umbilicus and the entire anterior bladder wall. Both the posterior bladder wall and both ureteric orifices can be seen with urine trickling out.
- Divarication of the recti.
- Complete epispadias.
- Wide separation of both pubic bones. This results in a short penis and a weak pelvic ring, and the child walks by waddling like a duck with nonunion of both pubic roots leading to a short pelvis.
Complications:
- Columnar metaplasia of the exposed bladder urothelium forms chronic irritation. There is a high incidence of malignant transformation resulting in adenocarcinoma of the bladder.
- Ascending infection to the kidneys. Bilateral chronic pyelonephritis is the most common cause of death.
- Contracted bladder plate.
Treatment:
- Immediate complete reconstruction within 72 hours of labor.
- Staged reconstruction.
- Excision of unhealthy contracted bladder plate with urinary diversion.
2. Posterior Urethral Valve
Definition:
The presence of urothelial (mucosal) folds in the form of valves just distal to the verumontanum. The valves cause high resistance to the outflow of urine from the bladder to the outside during voiding, but easily allow passage of urinary catheter.
Clinical Picture:
- Antenatal US: Prenatal bilateral hydronephrosis with a full bladder and dilated posterior urethra (keyhole sign) during the last trimester of pregnancy, and oligohydramnios.
- Postnatal.
- Obstructive urinary symptoms.
- Recurrent UTI.
- Sepsis.
- Renal failure.
Diagnosis:
1. Voiding cysto-urethrogram (VCUG):
- The urethra proximal to the valves appears dilated.
- The bladder is usually huge.
- Bilateral reflux with bilateral hydroureteronephrosis.
2. Endoscopy: the valves are visualized by urethroscopy.
Complications:
- Evidence of obstructive uropathy in the bladder (trabeculation, diverticula, chronic retention).
- Evidence of obstructive uropathy in the upper system (bilateral hydroureter and hydronephrosis).
- Urinary Tract infection.
- Renal insufficiency.
Treatment:
- Early presentation during antenatal care or at the first day after delivery: evacuation of the bladder by a urethral catheter then endoscopic valve incision or fulguration.
- Late presentation with the development of complications is usually treated by cystostomy or ureterostomy and treatment of complications e.g. treatment of sepsis.
3. Hypospadias
Definition:
Hypo = below, Spadias = meatus.
Congenital failure of the fusion of the urethral folds to form the urethral tube leads to the urethral meatus misplaced proximal to the tip of the glans penis along the ventral surface of the penis.
It includes:
- The prepuce appears incomplete. It covers the dorsum of the penis only giving the impression that the baby was born partially circumcised with ventrally lost skin.
- In severe cases of hypospadias, there is ventral curvature of that portion of the penis lined by the urethral plate. The curvature is known as “chordee” and is caused by a relatively short urethral plate that causes a bow-string appearance of the penis.
Types:
- Glanular hypospadias: urethral meatus is inside the glans penis. It is the commonest and mildest form of hypospadias.
- Penile hypospadias: urethral meatus is at any level of the shaft of the penis.
- Penoscrotal hypospadias: The urethral meatus is at the penoscrotal junction.
- Scrotal hypospadias: The urethral meatus is at the scrotum.
- Perineal hypospadias: The urethral meatus is in the perineum behind the scrotum. A bifid scrotum is always present in this condition. It is the rarest and most severe form of hypospadias and is always associated with severe chordee.
Complications:
The more proximal is the urethral meatus, the more severe are the complications.
- In glanular hypospadias, there is no real complication except for slight disfigurement.
- In perineal hypospadias, disfigurement is extreme, there is the inability to direct the urine stream during micturition, and there is the inability to penetrate the vagina during intercourse because of the severe chordee.
Principle of Surgical Correction: starts from 6 months of age.
A new urethral tube is created at the site of the absent urethra (along the area that corresponds to the urethral plate). This procedure should be preceded by the excision of the chordee if present. Most cases of hypospadias repair are done in 1 stage. However, a 2-stage repair is resorted to in complicated cases. The surgical techniques of hypospadias repair are not required from the medical student.
4. Epispadias
Epi above, spadias meatus
A very rare anomaly where the urethral meatus is misplaced proximal to the tip of the glans penis along the dorsal surface of the penis.
Types:
- Incomplete epispadias: failure of closure of the dorsal wall of the urethra from the tip of the glans penis to a level distal to the external sphincter.
- Complete epispadias: failure of closure of the dorsal wall of the urethra from the tip of the glans penis to the bladder neck. The urinary sphincters are poorly developed always resulting in incontinence of urine. Complete epispadias is always present with ectopia vesicae (bladder exstrophy).
Treatment:
Surgical repair follows the same principles as of hypospadias repair. The results are more disappointing with a complete epispadias.
Cryptorchidism
Embryology: In early embryonic life, the testicles are located retroperitoneally in the abdomen. At the end of the 7th month, they move distally along the inguinal canals to reach their final destination in the scrotum at full term.
Physiology: The testicles are heat-sensitive organs. Normal spermatogenesis is possible only when the testicles are at room temperature. This is why they are located in the scrotum. An undescended testis (inguinal or intra-abdominal) is present in body temperature. This is considered a high temperature that impeded normal spermatogenesis, and can result in infertility if the condition is bilateral.
Types:
- Palpable or impalpable.
- According to clinical examination.
- Undescended testis: arrest of testicular descent along its normal course to the scrotum. An undescended testis is present either in the inguinal canal (90%) or in the abdomen (10%).
- Ectopic testis: testicular descent takes an abnormal course, the commonest being in the superficial inguinal pouch (superficial to the external oblique aponeurosis).
Etiology:
- Undescended testis: a short vascular pedicle (usually unilateral); deficiency in gonadotrophin hormone secretion (rare, and always bilateral).
- Ectopic testis: abnormal connection of the gubernaculum.
Diagnosis
1. Clinical examination:
- Absence of the testis from the scrotum (empty scrotum).
- It can be clinically palpable if in the inguinal canal close to the external ring or if it is ectopic in the superficial inguinal pouch.
2. Laparoscopy: If the testis is never clinically palpable and intra-abdominal.
3. Radiology: MRI and US (rarely conclusive).
4. Laboratory: Karyotyping and hormonal assay if bilateral impalpable testes.
Complications:
- Irreversible spermatogenic arrest by 1 years of age from testicular atrophy caused by body temperature (too high for the testis). Infertility occurs if the condition is bilateral and left untreated after I year of age.
- The risk of malignancy in the abdominal undescended testis is higher than in the scrotal testis.
Treatment:
If impalpable: laparoscopy is indicated to search for the testis inside the abdomen. The testis may vanish, atrophic, small, or normal. Trial of descend in one or two stages is done for normal testis.
If palpable:
- Early age, preferably before 1 year of age: usually inguinal orchiopexy (the testis is exposed, dissected, and mobilized to its normal scrotal position where it is fixed).
- Late age when there is evidence of testicular atrophy: orchiectomy (done to guard against the high risk of malignancy in the undescended testis).
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
What are urinary tract infections?, kidney problems, Urinary retention and Bladder stones
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism
Histological structure of kidneys, Uriniferous tubules and Types of nephrons
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption and secretion
Urinary passages function, structure of Ureter, Urinary bladder & Uvulae vesicae
Urinary system structure, function, anatomy, organs, Blood supply and Importance of renal fascia
Urinary bladder structure, function, Control of micturition by Brain & Voluntary micturition