Methods of diagnosis of genetic variants, Ethical and social issues related to genetic testing
Genetic testing looks for mutations or variants, in your DNA, It is useful in many areas of medicine and it can change the medical care you or your family member receives, It can provide a diagnosis for a genetic condition such as Fragile X or information about your risk to develop cancer, There are many different kinds of genetic tests.
Methods of Diagnosis of genetic variants
1. At the DNA/gene level
- If a mutation is known to be a common cause of the disease then a targeted molecular test. PCR-based, can be rapidly used to test for the presence or of this mutation (e.g. common mutation of a single base such as in sickle cell anemia).
- If there are several mutations or if no specific mutation is commonly involved in a certain disease then a whole gene sequencing (Sanger sequencing 1-10Kb) is performed and variants detected will be analyzed and interpreted according to variant characteristics to categorize if it is polymorphism (with a benign effect) or disease-causing (pathogenic).
- If there are several genes causing the same disease, then a targeted panel can be deep sequenced by next-generation sequencing (1Mb).
- If the above is not applicable or were not conclusive for diagnosis then a wider genome analysis can be undertaken by whole exome (1.5% of the genome 45Mb) or whole genome sequencing (3Gb) using next-generation sequencing
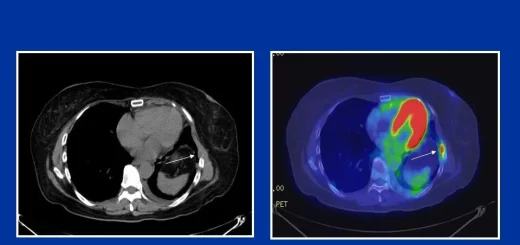
- If the mutation is a large sequence, it can be detected at a chromosomal level using molecular cytogenetics such as FISH (using probes for specific chromosomal loci or genes to test for deletion or amplifications (copy number variants) and if several chromosomal defects or rearrangements are suspected such as in cancer then spectral karyotype can be used, If specific chromosomal loci are to be tested for gains or losses then comparative genomic hybridization can be used.
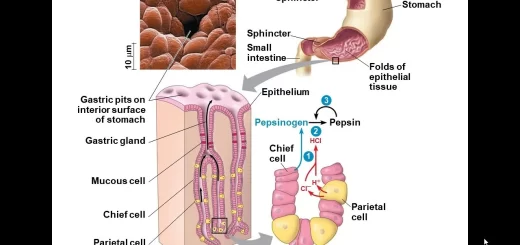
2. At the RNA to test for gene expression
- For a single gene expression: RT PCR (reverse transcriptase PCR) in which the expressed mRNA in the tissues will be converted to complementary DNA by reverse transcriptase enzyme followed by amplification using PCR and detected by a qualitative method such as gel electrophoresis or quantitatively by real-time PCR.
- All expressed RNA from specific cells or tissue can be also analysed to determine under or over-expression of genes. This is called Transcriptomics.
- Analysis of micro RNA can give an idea of the regulatory mechanisms of gene expression.
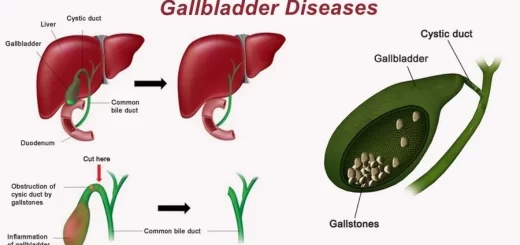
3. At the Protein level:
- Through the study of protein-protein interaction to determine pathways and changes occurring if a particular protein is mutant.
- Functional assays to experimentally determine a certain protein function and compare the normal function versus the effect of the mutation.
- Knock-out mice are experimental animal studies to determine the effect of a particular gene loss of function.
Molecular Genetic Diagnosis
Clinical Applications of Molecular Genetics: Molecular analysis is potentially possible for any single gene disorder and the list of disorders that can be diagnosed by molecular methods is increasing every day.
- Direct mutation analysis: When a genetic variant is detected in a proband this allows a specific test to be applied to relatives. This is particularly helpful for carrier detection. N.B presence of the mutation does not make a clinical diagnosis because many disorders have reduced penetrance, in which case the test is considered as a presymptomatic test.
- Linkage analysis: used for conditions which have been mapped to a certain locus and the causative gene is linked to DNA markers such as repetitive sequences (microsatellites). This is used if the gene itself is unknown or in case of limitation to identify a specific mutation. In this case, the segregation of the disease allele within the family is studied by being linked to DNA markers.
Indications of Molecular Testing
1. Carrier detection
DNA abnormalities are readily detected in the heterozygous state, therefore reliable in carrier detection e.g. Duchenne Muscular Dystrophy (X-linked) which unlike the enzyme level (serum Creatine Kinase) will not be affected by the X chromosome inactivation.
2. Prenatal diagnosis
DNA is not usually altered during embryonic development and therefore can be used in early prenatal diagnosis in the first trimester from chorionic villus sampling, and there is the potential for preimplantation detection.
3. Presymptomatic diagnosis
This is not related to disease onset since it is based on the detection of mutations in the DNA. It is used for late-onset diseases e.g. Huntington disease and familial cancers.
4. Diagnostic genetic testing
For specific mutations, testing is feasible for clinical disorders, suggesting a particular genetic disorder e.g. hereditary breast cancer, however, the individual must know that the test is indicated for suspicion of a genetic disease and this will affect the risk of other family members, it is also important to use tests relevant to the disorder concerned in the testing e.g. patient complaining from headache in a family with Huntington disease if tested for Huntington disease is considered as presymptomatic testing and consent has to be obtained before testing.
5. Molecular testing
Molecular testing can explain the variability of expression of a certain disorder mostly exemplified by disorders caused by expansion of trinucleotide repeats e.g. myotonic dystrophy, fragile X.
6. Medicolegal testing
Medicolegal testing, zygosity testing, and disputed paternity using DNA fingerprinting.
Ethical and social issues related to genetic testing
- Genetics affect the whole family and society in general not just the individual undertaking the test.
- Genetic counselling is not directive, non-judgemental communication between the medical geneticist and the patient or the consultand.
- Informed consent before genetic testing (predictive).
- Confidentiality (sensitivity to stigmatisation).
Examples of ethical dilemmas related to genetic testing
- Antenatal diagnostic testing: termination of pregnancy is only justified for serious disorders causing lifelong pain and suffering, but there is concern over wider non-ethical application.
- Predictive testing in childhood: parents sometimes wish to know if their children have inherited the gene of an AD disorder that develops late in adulthood and is present in the family e.g. Huntington Disease (HD). For conditions in which no treatment is available the testing should be postponed till the child grows and decides for him/herself, it should be respected that the child has the right to make his or her informed decision at the age of 18 years.
- Implications of predictive testing on immediate relatives: predictive testing for an adult onset disease such as HD may be requested by a young 20-year-old adult whose grandparent is showing manifestations suggestive of this disorder; however his father does not show the clinical picture of the disease and does not wish to know. It is acceptable that the right of the young adult to know should have priority over the right of the parent not to know.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Off-target effect of drugs types, Role of Precision Medicine and Pharmacogenetics
Genetics variants effects, Types of polymorphisms and disease-causing mutations
Polygenic inheritance vs Single gene inheritance, Non-mendelian inheritance and Genomic imprinting
Chromosomal disorders, structure, classification, and Types of numerical chromosomal abnormalities
Genes, Chromosomes, Proteins, Bacteriophages & Quantity of DNA in the cells
Packaging of DNA, Genome, chromosomal proteins, DNA in Prokaryotes & Eukaryotes