Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
The tongue is anchored to the mouth by webs of tough tissue and mucosa, It is vital for chewing and swallowing food, as well as for speech, It has many nerves that help detect and transmit taste signals to the brain, It is a muscular organ in the mouth, It is covered with moist, pink tissue called mucosa, Tiny bumps called the papillae give the tongue its rough texture.
Tongue
It is a mass of striated muscles covered with mucous membranes.
Parts: It is formed of tip + dorsal and ventral surfaces + root.
Mucous membrane of the tongue
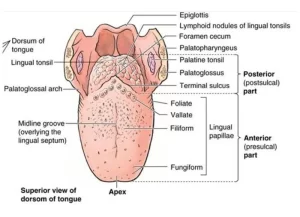
The dorsal surface of the anterior two-thirds (oral part) is separated from the posterior third (pharyngeal part) by a V-shaped sulcus, the sulcus terminalis, The apex of the sulcus is marked by a small pit (the foramen caecum).
The anterior two-thirds dorsal surface is covered with papillae (filiform, fungiform, and vallate), While the posterior third of the anterior surface is devoid of papillae and contains aggregations of lymphoid tissue (lingual tonsil).
The mucous membrane of the inferior surface of the tongue is smooth and reflected to the floor of the mouth, and it is connected to it by the frenulum, On both sides lie the lingual artery, lingual nerve, and deep lingual vein (from medial to lateral), Lateral to the lingual vein the mucous membrane forms a fringed fold (plica fimbriata).
Muscles of the tongue
The muscles of the tongue are divided into two types:
Intrinsic muscles
They are confined to the tongue and not attached to the bone, They are supplied by the hypoglossal nerve, They change the shape of the tongue by narrowing the tongue (by transverse muscle), shortening (by longitudinal muscle), and thinning (by vertical muscle).
Extrinsic muscles
They change the position of the tongue:
1- Styloglossus muscle:
- Origin: Styloid process of the temporal bone.
- Insertion: The side of the tongue.
- Nerve supply: Hypoglossal nerve.
- Action: It draws the tongue upwards and backwards.
2. Palatoglossus muscle: It is described with the palate.
3. Genioglossus muscle: It is a flat fan-shaped muscle that lies close to its fellow on the opposite side.
- Origin: Superior genial tubercle of the mandible.
- Insertion: The whole length of the tongue.
- Nerve supply: Hypoglossal nerve.
- Action: With the opposite muscle, it protrudes the tongue. They also depress the median part of the tongue.
4- Hyoglossus muscle: It is a quadrilateral muscle.
- Origin: It takes origin from the lateral part of the body and the whole length of the greater horn of hyoid bone.
- Insertion: It is inserted into the side of the tongue lateral to the genioglossus muscle.
- Nerve supply: Hypoglossal nerve.
- Action: Depression of the tongue.
Nerve supply of the tongue
1- Sensory nerve supply:
- General sensation: It is through the lingual nerve to the anterior two-thirds of the tongue. The posterior third is supplied by the glossopharyngeal nerve.
- Taste sensation: It is carried by the chorda tympani to the anterior two-thirds, and by the glossopharyngeal nerve to the posterior third. General and taste sensations of the most posterior part of the tongue are carried by the internal laryngeal branch of the vagus nerve.
2- Motor innervation:
All muscles of the tongue are supplied by the hypoglossal nerve, except the palatoglossus muscle which is supplied by the cranial part of the accessory nerve through the pharyngeal plexus.
Arterial supply of the tongue
- Lingual artery.
- Tonsillar branch of facial artery.
- Ascending pharyngeal artery.
Venous drainage of the tongue
The lingual vein which drains into the internal jugular vein.
Lymphatic drainage of the tongue
- The tip and frenulum of the tongue drain into submental lymph nodes.
- The peripheral lymphatics from the anterior two-thirds pass to the submandibular lymph nodes. Some pass directly to the upper and lower deep cervical lymph nodes.
- The central lymphatics from the anterior two-thirds drain mainly to the deep cervical lymph nodes and a few pass to the submandibular lymph nodes. They drain to both sides.
- Lymphatics from the posterior third of the tongue drain into deep cervical lymph nodes of both sides.
Histological structure of the lip
The lips are the entry point of the alimentary canal, In a longitudinal section, three surfaces of the lip are histologically distinguishable:
- The skin surface: formed of hairy thin skin.
- The red margin: It is a transitional zone between the skin and the oral mucosa of the lip which is richly supplied by sensory nerve endings. It is covered by thin keratinized stratified squamous epithelium. The epithelium is indented by long connective tissue papillae. The red color of the lip-free margin is due to the reflection of the numerous blood capillaries in the underlying connective tissue papillae.
- The mucous surface: It is lined by the oral mucosa (non-keratinized stratified squamous epithelium). The lamina propria contains mucous acini of the labial salivary glands with their ducts open into the vestibule, keeping this surface moist. The main bulk of the lip is formed of striated muscle fibers (the orbicularis oris muscle) among fibro-elastic connective tissue rich in fat cells.
Histological structure of the tongue
The tongue is a muscular organ adapted for food manipulation, speech, general sensory perception and the special sensory function of taste. The main bulk of the tongue is formed of striated muscle fibers (intrinsic lingual muscles) which run in three directions: longitudinal, transverse, and vertical (at right angles to each other). They are embedded in loose and adipose tissue to allow maximal mobility of the tongue.
The ventral surface is lined by the oral mucosa, loosely attached to the underlying tissue to permit free bending and mobility of the tongue. The dorsal surface is divided by the V- shaped gustatory line (sulcus terminalis) into anterior 2/3 and posterior 1/3. The mucosa of the anterior 2/3 of the dorsum of the tongue (papillary surface) is firmly attached to the underlying tissue and is modified to form a large number of lingual papillae.
The lingual papillae are elevations on the anterior 2/3 of the dorsal surface of the tongue. They increase the surface area of the lingual mucous membrane coming in contact with the food. Each papilla is covered by stratified squamous epithelium and has a core of connective tissue lamina propria that projects to indent the epithelium thus forming secondary papillae.
Types of lingual papillae
1. Filiform papillae
- Number: most numerous.
- Distribution: arranged in rows, parallel to the gustatory line over the anterior 2/3 of the dorsal surface of the tongue.
- Shape: conical with antero-posterior inclination.
- Taste buds: absent.
2. Fungiform papillae
- Number: few.
- Distribution: scattered among the filiform papillae being more numerous on the tip and edges of the tongue dorsum.
- Shape: mushroom-shaped with a rounded summit and narrow base. They have vascular connective tissue core; so seen as red spots in the living state.
- Taste buds: few, present in the epithelium on the summit of the papilla.
3. Circumvallate (vallate) papillae
- Number: from 8-12 papillae in the human tongue.
- Distribution: aligned just in front of the gustatory line.
- Shape: the largest, seen by the naked eye. They are triangular in shape, embedded within the substance of the tongue, and project for a short distance above the surface. Each papilla is surrounded by a trench where ducts of Von Ebner’s glands open into its bottom.
- Taste buds: numerous, present along the sides of the papillae.
4. Foliate papillae
- Number: not recognized in adult human but developed in rabbit.
- Distribution: arranged in rows, on the lateral sides of the tongue.
- Shape: rectangular with parallel sides.
- Secondary papillae: long.
- Taste buds: numerous, present along the sides of the papillae.
Von Ebner’s glands
These are the serous lingual salivary glands found in the connective tissue lamina propria encircling each circumvallate papilla. Their ducts open at the bottom of the trenches surrounding these papillae.
Function:
- Their serous secretion dissolves the food particles to facilitate the perception of taste.
- The flow of secretion is important for washing away food particles from around the taste buds so that they can receive new gustatory stimuli.
Clinical hint:
The keratinized epithelium of the filiform papillae is continuously shed in saliva. In gastrointestinal disturbances and in fevers the shedding of the epithelium is delayed and it accumulates in a layer mixed with bacteria to form a grey film over the surface of the tongue. This is called the coated tongue.
The taste buds
The taste buds are neuroepithelial structures specialized for the perception of taste sensation.
Sites
They are embedded within the epithelium of the lingual papillae; namely the fungiform, the foliate and the circumvallate papillae. Limited numbers of taste buds are present within the epithelium covering the palate and epiglottis. In histological sections, they appear as pale, ovoid structures, oriented at the right angle to the lining epithelium and connected to the surface of the epithelium by a small opening called the taste pore (gustatory pore).
Types of cells in taste bud
- Supporting cells.
- Neuroepithelial (gustatory) cells: spindle-shaped and associated with the afferent gustatory nerve fibers. They have long, apical microvilli (gustatory hairs) which protrude out into the taste pore. Tastants (food dissolved in saliva) stimulate the gustatory hairs of the neuroepithelial cells.
- Basal cells: small, pyramidal cells located between the bases of the other cells. They are stem cells that can divide and differentiate replacing the taste cells almost every 10 days.
You can download the application on google play from this link: Science online Apps on Google play
Git function, Types of salivary secretion & Composition of saliva
Histological structure of salivary glands, Parotids, Sublingual and Submandibular glands
Norma lateralis features & anatomy, Mandible surfaces, nerves & ligaments
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Salivary glands function, shape, lobes, surfaces and Structures within the parotid gland