Git function, Types of salivary secretion and Composition of saliva
The alimentary canal is the doorway through which all nutrients and energy sources pass before they are utilized. It extends from mouth to anus. The associated glands include salivary glands, liver and pancreas which empty their secretion into the alimentary canal. Accessory organs include the tongue, teeth, and muscles of mastication.
Parts of the digestive system
- Alimentary canal.
- Associated glands.
- Accessory organs.
Physiological functions of the GIT
- Digestion: is the breakdown of food materials into small particles, ready for absorption and utilization by the body cells. Digestion mostly occurs in the proximal part of the small intestine.
- Absorption is the transfer of the contents of the gut from the lumen into the mucosa.
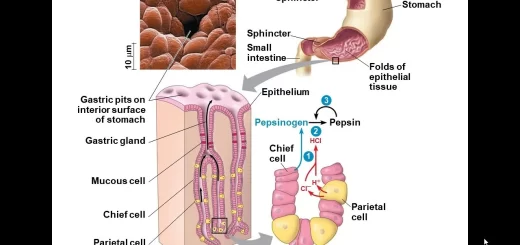
- Secretion: It is the transport of fluid, electrolytes, and peptides (etc) from blood, to the lumen of the GIT. About 7500 ml of secretions are added daily to the lumen of the GIT. Secretions are usually isotonic with the plasma, except for saliva which is hypotonic relative to the plasma.
- Immune function: Humoral antibodies and cellular immune system (lymphocytes in the Peyer’s patches of the intestine) protect the body against micro-organisms in the lumen of the gut.
- Endocrine function e.g. release of somatostatin, intestinal glucagon, gastrin, secretin, and cholecystokinin.
Innervation of the digestive tract
Except for the striated muscles of the mouth, the upper part of the oesophagus, and the external anal sphincter, the musculature of the digestive tract is composed of smooth muscle fibers. All smooth muscles are involuntary, and nervous control in the GIT takes place by autonomic nerves which are both extrinsic (sympathetic and parasympathetic) and intrinsic (enteric nerve plexus).
Intrinsic innervation of the gut
The enteric nerve plexus comprises:
- The myenteric (Aurbach’s plexus): lies in the musculosa between the circular and longitudinal muscle layers. It is concerned with controlling the motor activity of the alimentary canal. It is mainly excitatory to the tonic and rhythmic contractions, but it also contains some inhibitory neurons.
- The submucosal (Meissner’s plexus): lies in the submucous layer. It is concerned with controlling the local secretory function of the GIT by stimulating the local exocrine and endocrine secretory cells. It contains the neurons of the sensory afferent nerves which arise from the mucosal layer.
Extrinsic innervation of the gut
The intrinsic neural plexuses of the enteric nervous system are connected together and are modulated by extrinsic autonomic nerves (sympathetic and parasympathetic). The parasympathetic supply is generally excitatory to the enteric nervous system: it stimulates motility and secretion. However, it contains also some inhibitory vagal fibers to the stomach and the gastrointestinal sphincters.
The sympathetic nerve supply generally inhibits secretion and motility. However, it contains also some excitatory fibers. Sensory fibers arise from the luminal epithelium and wall of the gut to the enteric plexuses and from there to the prevertebral ganglia, spinal cord, and brain stem.
Salivary secretion
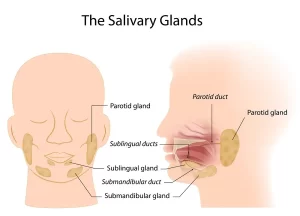
There are three main pairs of salivary glands, which are the parotid, submandibular and sublingual salivary glands. In addition, the buccal mucosa contains a large number of small glands which secrete mucus. Salivary glands are exocrine glands, with ducts opening into the oral cavity. The volume of salivary secretion ranges between 1000 and 1500 ml/day.
Types of salivary secretion
- Serous secretion: containing the enzyme ptyalin (α-amylase) which is an enzyme for starch digestion.
- Mucous secretion: containing mucin which is a glycoprotein. This type of secretion renders the salivary secretion viscous for protective and lubricating purposes.
In man, the parotid secretion is entirely of the serous type. The submandibular glands secrete both serous and mucus types of secretion and the sublingual as.
Gland Type of secretion % of total salivary secretion in human (Total 1.5 L/day)
Parotid Serous 25
Submandibular Mixed 70
Sublingual Mucous 5
Salivary secretion is an active process
The composition of saliva cannot be explained by a simple process of filtration because it is not identical to the composition of the plasma. Modification of saliva occurs during its passage in the duct system under the effects of aldosterone which causes reabsorption of Na+ in exchange with K+ and H+.
Thus saliva is the hypotonic solution. Thus salivary secretion does not obey the laws of physical chemistry and needs energy for the manufacture of its constituents as well as for the osmotic or mechanical work done. During salivary secretion, the oxygen consumption of the glands increases 3-4 times the resting value, and glucose uptake by the gland is also increased.
Innervation of salivary glands
Salivary glands are supplied by the autonomic nervous system. Salivary secretion is a complementary function between the sympathetic and parasympathetic nervous systems.
Effects of stimulation of parasympathetic nerve supply
Stimulation of the parasympathetic nerve supply causes the production of the chemical transmitter acetylcholine at the postganglionic nerve endings, which has secretory and vasodilator effects which result in:
- Profuse secretion of watery saliva with a natively low content of organic material (enzymes, mucin) and has some electrolytes.
- Pronounced vasodilation: blood flow increases up to ten times during activity and oxygen consumption increases about 3 folds.
Effect of stimulation of the sympathetic nerve supply
- Release of small amounts of viscid saliva rich in organic constituents only in the submandibular and sublingual glands.
- Marked vasoconstriction and reduction of the blood flow.
Composition of saliva
The amount of salivary secretion ranges from 1 to 1.5 liters/day. It is a colourless, viscous fluid, with slightly acidic pH: 6.6-7.1. It is hypotonic relative to the plasma.
Saliva contains
- 99.5% water
- 0.2% inorganic constituents.
- 0.3% organic solids.
I. Inorganic constituents:
- NaCl and KCI: these chloride ions act as coenzymes for salivary amylase.
- H2CO3, NaHCO3, NaH2PO4, and Na2HPO4: these bicarbonate and phosphate buffer systems help to neutralize acids or alkalies introduced into the mouth.
- Calcium salts as calcium bicarbonate and phosphate. Calcium ions are needed to activate salivary amylase. If the pH of saliva is increased (alkaline) by the loss of CO2 to the atmosphere. precipitation of insoluble calcium salts on teeth occurs and forms with organic matter a crust known as tartar. If calcium salts are precipitated in the duct system salivary calculi results.
- Potassium thiocyanate which is formed from the metabolism of proteins. It has a bactericidal action.
II. Organic constituents:
i. Ptyalin (a-amylase), lysozyme and lingual lipase. Salivary amylase acts at an optimum pH of 6.9-7.1. It hydrolyses cooked starch only because raw starch granules have a cellulose covering. Cooking favors digestion because it breaks the cellulose wall and in turn facilitates the action of salivary amylase. The action of salivary amylase continues in the stomach for about half an hour until gastric HCI lowers the pH of the medium.
Lysozyme: has antibacterial action because it destroys the polysaccharides covering of bacterial capsule.
ii. Albumin, globulins, mucin, and traces of urea, uric acid, and lactic acid.
iii. Epidermal growth factors.
Functions of saliva
- Moistens food to facilitate its swallowing.
- Cleans the mouth by: a mechanical wash of the food residues and the shed epithelial cells which prevents putrefaction. Antibacterial action by lysozyme, and the bactericidal effect of thiocyanate ions. saliva contains protein antibodies that can destroy the bacteria in the oral cavity.
- Facilitates speech by moistening of the oral cavity which includes the soft palate, tongue, and lips.
- Has a role in the digestion of starch by salivary amylase. Digestion of starch is completed by pancreatic amylase.
- Dissolves some food materials to facilitate its stimulating effect on taste buds (helps taste sensation).
- Has a role in water balance because the dryness of the buccal and pharyngeal mucosa initiates the sensation of thirst.
- Has a buffering action via its content of bicarbonates, phosphates, and mucin, to protect the buccal cavity from excessive acids or alkalis. Excessive alkalis lead to precipitation of calcium salts around the teeth which forms with organic matter hard concretions called tarter, bacteria flourish underneath the Tartar leading to chronic inflammation of the gums. Excessive acids dissolve enamel and dentine of teeth after prolonged exposure.
- Protects against irritating substances and neutralizes excessively cold or hot food.
- Helps in body temperature regulation in animals with no sweat glands (e.g. dogs) by evaporation of saliva.
- Excretes iodides and mercury which may produce inflammation of buccal mucosa (stomatitis). Also, in lead poisoning a blue line formed at the margins of teeth and gums. Urea is excreted in saliva in renal diseases and some little glucose may be also excreted in diabetes mellitus. This excretory process is not very effective because these materials are swallowed again.
Control of salivary secretion
Salivary secretion is evoked by a nervous mechanism. Hormonal regulation would be too slow to meet with such a function which needs a rapid response. It plays a role only in the modification of salivary contents. Nervous regulation is achieved via two types of reflexes conditioned and unconditioned.
A- Unconditioned reflexes (Inborn, do not depend on training)
Unconditioned reflexes are triggered if food, acids or alkalis are introduced into the mouth, stimulating the buccal mucosa mechanically or chemically. This leads to profuse salivation. Also, any irritation of the buccal cavity by moving the tongue inside the mouth or during speech causes salivary secretion.
Receptors
- The four types of taste receptors in the tongue namely salt, acid, sweet, and bitter receptors.
- Thermoreceptors and pain receptors in the buccal cavity.
- Pharyngeal and oesophageal receptors.
Afferent
Impulses for taste sensation from the anterior two-thirds of the tongue are conducted by the chorda tympani branch of the facial nerve. From the posterior third of the tongue and pharynx impulses for taste sensations are carried by the glossopharyngeal and vagus nerves.
Impulses from mechanical stimuli and common sensations (touch, pain, warm, and cold) are conducted by the lingual nerve, palatine branch of the trigeminal nerve and pharyngeal branch of the vagus nerve.
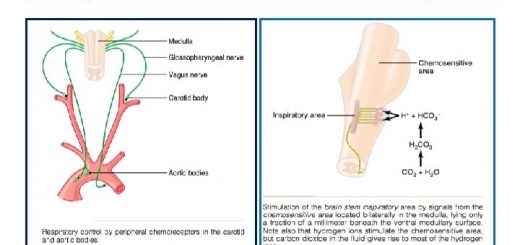
Centre: Parasympathetic: salivatory centers in the medulla oblongata. Sympathetic: lateral horn cells in the first and second thoracic segments of the spinal cord.
Efferent: Along the autonomic nerves supplying the salivary glands.
Effectors: Salivary glands.
Response: Salivary secretion
Sympathetic: produces a viscid organic secretion.
Parasympathetic: produces a watery secretion.
B- Conditioned reflexes (acquired, depend on training)
Stimulation of any sensory nerve endings in the body in absence of food from the buccal cavity (as optic, auditory, and olfactory nerves) can be converted by training into conditioned stimuli for salivation.
This is documented by the classic experiment by Pavlov, who used to ring a bell before giving food to a dog. Subsequently, ringing the bell without any food intake triggered salivation in the dog. In this case, hearing the bell is associated in the cerebral cortex with food intake.
Receptors: Lie in the relevant sense organ, e.g. in eye, nose…
Afferent: Afferent of sense organs e.g. Optic nerve, olfactory nerve,….
Centre: Cerebral cortex and from there the impulse travels to the salivatory centres in the medulla oblongata.
Efferent: Nerve supply to salivary glands.
Effectors: Salivary glands.
Response: Salivary secretion.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Histological structure of salivary glands, Parotids, Sublingual and Submandibular glands
Norma lateralis features & anatomy, Mandible surfaces, nerves & ligaments
Salivary glands function, shape, lobes, surfaces and Structures within the parotid gland
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Tongue function, anatomy & structure, Types of lingual papillae & Types of cells in taste bud