Suprarenal glands (adrenal glands) anatomy, structure and Effect of Deficiency of Catecholamines
The adrenal glands lie at the superior poles of the kidneys, Each gland is composed of two distinct parts, the adrenal medulla, and the adrenal cortex, The adrenal medulla is functionally related to the sympathetic nervous system, it secretes the hormones epinephrine and norepinephrine in response to sympathetic stimulation, The adrenal cortex secretos steroid hormonet.
Anatomy of Supra-renal glands (adrenal glands)
The adrenal gland lies at the upper pole and adjacent part of the medial border of the kidney. The right one is triangular while the left one is semilunar in shape.
Relations:
- Posteriorly: the diaphragm.
- Postero-inferiorly: the kidney.
- Medially: the celiac ganglion.
- Anteriorly: the right one is partially covered by the peritoneum and related to the IVC and the liver. The left one is covered by the peritoneum of the lesser sac and forming part of the stomach bed. Its lower border is related to the body of the pancreas and splenic vessels.
Arterial supply:
Each gland is supplied by three arteries:
- Superior supra-renal artery (from an inferior phrenic artery).
- Middle supra-renal artery (from the abdominal aorta).
- Interior supra-renal artery (from the renal artery).
Venous drainage:
Each gland is drained by a single vein: The right supra-renal vein drains into the IVC, The left supra-renal vein drains into the left renal vein.
Structure of suprarenal gland
Each gland consists of 2 parts:
- The cortex: the yellow peripheral layer, which lies beneath the capsule. It originates from the mesoderm, the same origin as the endocrine cells of the gonads secreting steroid hormones. The cortex constitutes nearly 80-90% of the gland.
- The medulla: the reddish-brown central layer, which lies deep to the cortex. It originates from the neural crest. it has the same origin as the sympathetic nervous system; hence médulla is considered as a modified sympathetic ganglion, where the neurons have acquired an endocrine activity and secrete catecholamines.
Histological structure of the Suprarenal gland
- The stroma: the gland is covered by a connective tissue capsule that sends thin septa inside the gland. A network of reticular fibers supports the secretory cells and the blood vessels of the cortex and medulla.
- The parenchyma is divided into 2 histologically and functionally different regions; the cortex and the medulla.
Suprarenal medulla
It forms the central part of the suprarenal gland. As it develops from the ectodermal neural crest, it contains two populations of parenchymal cells:
- Chromaffin cells: their function is the synthesis and secretion of catecholamines.
- Sympathetic ganglion cells are scattered throughout the medullary tissue. They modulate the secretory activity of the suprarenal cortex and innervate is blood vessels.
Chromaffin cells (Pheochromocytes)
By LM: These are called chromaffin cells due to the affinity of catecholamines granules (epinephrine and nor-epinephrine) in their cytoplasm to react with chromium salts and stain deep brown (chromaffin reaction). They are arranged in rounded groups or short cords intimately related to the medullary blood sinusoidal capillaries. The chromaffin cells are large ovoid cells with large spherical nuclei and pale basophilic cytoplasm.
By EM: The cytoplasm contains some profiles of rER, prominent Golgi complex, and secretory granules containing the catecholamines.
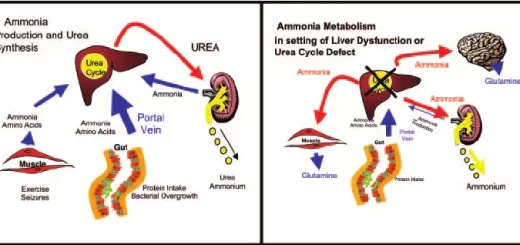
The medulla has a dual blood supply, arterial from the medullary arterioles and venous from the cortical sinusoids draining the cortex, Cortical glucocorticoids reaching the medulla are essential for the production of epinephrine by medullary chromaffin cells.
Action of Catecholamines
Catecholamines are secreted mainly in emergency conditions to support the actions of the sympathetic nervous system, They enable the body to perform extra work, These actions are produced through exerting the following effects:-
- Catecholamines increase the metabolic rate and O2 consumption leading to increased heat production.
- They stimulate glycogenolysis in the liver, so increase the blood glucose level.
- Catecholamines mobilize free fatty acids from adipose tissue, so their plasma level increased.
- Catecholamines directly increase both heart rate and its force of contraction, Norepinephrine produces vasoconstriction in most organs which increases both systolic and diastolic blood pressures.
- They cause splenic contraction which adds concentrated blood to the general circulation.
- They cause vasoconstriction to the renal blood vessels which may decrease urine volume.
- They increase the rate and depth of respiration by direct excitation of the respiratory centre and indirectly by increased metabolic rate, They cause bronchodilatation.
- Catecholamines potentiate skeletal muscle contraction and delay the onset of fatigue, They also cause vasodilation of skeletal muscle blood vessels.
- Catecholamines excite the nervous system and increase mental activity and alertness.
- They increase the visual fields.
Control of Secretion
Catecholamines secretion is low in basal states but is markedly increased during emergencies as a part of the diffuse sympathetic discharge, They are essential for preparing the body to withstand stresses as in muscular exercise, haemorrhage, hypoglycemia, and exposure to cold.
Effect of Deficiency of catecholamines
Unlike the adrenal cortex, the adrenal medulla does not appear to be essential to life, The adrenal medulla is nonessential because all its vital functions can be done by the activity of the sympathetic nervous system, There is no recognized syndrome of adrenomedullary insufficiency.
Effect of Excess catecholamines (pheochromocytoma)
- Hypertension is the dominant clinical manifestation of pheochromocytoma because it secretes adrenalin and noradrenalin). Hypertension might be sustained or episodic in paroxysms. Hypertension is associated with an increased risk of myocardial ischemia, congestive heart failure, renal injury, and cerebrovascular accidents. Sudden death may occur.
- Tachycardia.
- Palpitation.
- Hyperglycemia.
- Increase in basal metabolic rate.
Suprarenal (adrenal) cortex hormones, structure, function and location
Calcium metabolism, Calcitonin function, Vitamin D3 and Biosynthesis of calcitriol
Parathyroid gland anatomy, structure, function, hormones and Tetany types
Histological structure of thyroid gland and Functions of Thyroid Hormones (T3 & T4)
Endocrine system structure, function, disorders, Endocrine Glands and Hormones types