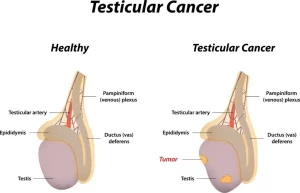
Diseases of testis and epididymis, Seminomas, Yolk sac tumors, Choriocarcinoma, Sex-cord stromal tumor
The male reproductive system consists of organs and glands involved in making offspring, These include the vas deferens, epididymis, prostate gland, penis, and testes, testes produce both sperm and androgens, primarily testosterone, Testosterone is controlled by the anterior pituitary luteinizing hormone, whereas the sperm production is controlled both by the anterior pituitary follicle-stimulating hormone and the gonadal testosterone.
Diseases of the testis
- Congenital: Cryptorchidism 1%
- Regressive. Atrophy.
- Inflammation: Mumps, GC, Chlamydia, E.Coli, Pseudomonas. TB
- Vascular diseases. Torsion.
- Tumors: Benign/Malignant, Germ Cell/non-Germ Cell.
Testicular atrophy
Atrophy is a regressive change that affects the scrotal testis and can have several causes:
- Atherosclerotic narrowing of the blood supply in old age.
- The end stage of inflammatory orchitis, whatever the etiologic agent (Mumps…).
- Genetic, Klinefelter syndrome.
- Cryptorchidism (undescended testis are sterile).
- Hypopituitarism.
- Generalized malnutrition or cachexia.
- Irradiation.
- Prolonged administration of antiandrogen therapy, as in the treatment of patients with carcinoma of the prostate.
Morphology
Classical pattern showing:
- ghosting or fibrosis of tubules.
- No spermatogenesis.
- Increased interstitial cells of Leydig.
Cryptorchidism
- 1% of all births.
- 10% bilateral.
- Most cases present with a palpable mass in the inguinal canal (second phase of descent).
- Complications: sterility- liable to trauma- increased incidence of germ cell tumors.
Normal testis shows tubules with active spermatogenesis, In Testicular atrophy in cryptorchidism, The tabules show Sertoli cells but no spermatogenesis, there is a thickening of basement membranes and an apparent increase in interstitial Leydig cells.
Testicular tumors
1. Seminomas
- The most common type of Germ cell t.
- Age: 3rd decade (never in children).
- Gross: bulky, fleshy mass, bulges above the surface.
- Microscopy: uniform seminoma cells forming lobules (nests)/ fibrous septa with lymphocytes.
- Cells are positive for PLAP/ CD117.
- Prognosis. Excellent.
- Treatment. Extremely radiosensitive.
- Tumor marker. Increased HCG in 10% of the cases (they may sometimes contain cyto and syncytiotrophoblasts that secrete HCG).
2. Embryonal carcinomas
- Age: 20-30 years.
- Behavior: More aggressive than seminoma.
- Gross. Bulky tumor with heamorrhage and necrosis.
- Undifferentiated tumors.
- Cells are CD30 positive.
- Metastasis, mainly heamtogenous.
- Tumor marker. AFP (mixed with yolk sac tumor) & HCG in 90% of the cases.
3. Yolk sac tumors
- Most common testicular tumor in children below 4 years of age.
- Microscopically: Characteristic schiller-duval bodies.
- Tumor marker: High serum AFP.
- Prognosis: Good prognosis in the young age group.
4. Choriocarcinoma
- Age: 20-30.
- Gross, small palpable nodule (even when extensively metastatic).
- Usually mixed.
- Microscopically: Tumor formed of cytotrophoblasts and
- syncytiotrophoblasts, No chorionic villi seen, heamorrhage and necrosis are present. (because the tumor grows too fast so it outgrows the blood supply).
- Behavior. A highly malignant form of testicular cancer
- Tumor marker: High serum HCG level.
5. Teratoma
- Age: Any age from infancy to adult life.
- Gross, Microscopic picture: Large bulky masses containing derivatives of endoderm, ectoderm and mesoderm.
- Behavior: In a child, it is usually benign… in adolescents and adult males, it is usually malignant.
6. Sex-cord stromal tumor
They are commonly benign functioning tumors.
- Leydig cell tumor: tumor cells look like Leydig cells. May secrete testosterone/oestrogen. Might have a clinical syndrome of hypertestosteronism, or sometimes even feminizing features. (gynecomastia, female hair distribution…..).
- Sertoli cell tumor: Tumor cells look like Sertoli cells.
Staging
- Tumor confined to the testis, epididymis, or spermatic cord.
- Distant spread is confined to retroperitoneal nodes below the diaphragm.
- Metastases outside the retroperitoneal nodes or above the diaphragm.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Enlarged prostate symptoms, Prostatic artery embolization (PAE) importance & risks
Prostate function, structure, lobes, Benign enlargement of prostate & malignant prostatic tumor
Nephroblastoma (Wilm’s tumor), Risk factors of Urothelial tumors (Tumors of transitional epithelium)
Urinary bladder structure, function, Control of micturition by Brain & Voluntary micturition
Urinary system structure, function, anatomy, organs, Blood supply & Importance of renal fascia
Histological structure of kidneys, Uriniferous tubules & Types of nephrons
Benign prostatic hyperplasia (BPH), TRUS biopsy, Prostate disease symptoms and treatment