Indifferent gonads, Development of gonads and genital ducts, Abnormalities of testis and ovary
However, the sex of the embryo is determined genetically at the time of fertilization, the gonads do not acquire male or female morphological characteristics until the seventh week of development, Gonads appear initially as a pair of longitudinal ridges, the genital or gonadal ridges, They are formed by the proliferation of the epithelium and condensation of underlying mesenchyme.
Indifferent gonads
Germ cells do not appear in the genital ridges until the sixth week of development, Before this time the sex gland is called the indifferent gonad”.
Sources
- Genital or gonadal ridge: The genital ridge lies on the medial side of the mesonephros. It gives the stroma of the gland.
- Coelomic epithelium: It consists of mesothelial cells (which line the coelomic cavity). They overly the genital ridge, proliferate & penetrate the underlying mesoderm forming the primitive sex cord of the indifferent gonad.
- Primordial germ cells: They are endodermal cells that arise from the wall of the yolk sac. They proliferate & Migrate along the dorsal mesentery of the hindgut to reach the genital ridge. They have an inductive influence on the development of the gonad into the ovary or testis.
Development of testes
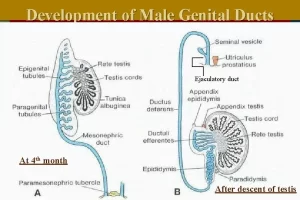
Steps of development:
- Under the influence of the SRY (sex-determining region on Y chromosome), which encodes the TDF (testis determining factor), the primitive sex cords continue to proliferate and penetrate deep into the medulla forming the testis (medullary) cords.
- Towards the hilum of the gland, the cords break up forming the tubules of the rete testis.
- Testis cords then lose their connection with the surface epithelium & become separated from the epithelium by a dense fibrous connective tissue (tunica albuginea).
- In the fourth month, the testis cords become horse-shoe-shaped, and their extremities are continuous with those of the rete testis, Testis cords are now composed of primitive germ cells and sustentacular cells of Sertoli derived from the surface epithelium of the gland.
The seminiferous tubules
Remain solid until puberty when they acquire a lumen. Their walls are composed of 2 kinds of cell:
- Sertoli cells are derived from the surface epithelium of the gland.
- Spermatogonia are derived from primordial germ cells.
Interstitial cells of Leydig
- Leydig cells are derived from the original mesenchyme of the gonadal ridge & lie between the testis cords.
- They begin the production of testosterone and the testis is able to influence sexual differentiation of the genital ducts and external genitalia.
- Finally, the rete testis becomes continuous with 15-20 mesonephric tubules which become the efferent ductules of the testis.
Descent of the testis
Testis developed in the abdomen. It descends to the scrotum. Gubernaculum testis (fibroelastic band) has 2 ends. One end is attached to the lower pole of the testis & the peritoneum of the peritoneal cavity. The other end of the gubernaculum testis is attached to the scrotum, Contraction of this band leads to a descent of the testis & part of the peritoneum. This part of the peritoneum is called the process vaginalis.
The testis invaginates the processes vaginalis, hence the testis is covered by visceral & partial layers of tunica vaginalis. The testis descends through the inguinal canal to reach the scrotum. After the testis reaches the scrotum the connection between the peritoneum & the processes vaginalis obliterates forming the vestige of processes vaginalis.
Factors controlling the descent of the lower pole of the testis
- Hormonal factors under the effect of the androgenic hormone, the testis descends.
- Descent occurs due to an increase in the intraabdominal pressure.
- Regression (contraction) of the gubernaculum testis.
Abnormalities
- Incomplete descent of the testis: the testis may be found in the inguinal canal for example.
- Ectopic testis: the testis is found in abnormal sites: in the perineum, in the abdominal wall.
- Hydrocele: due to failure of obliteration of the connection between the peritoneum & the processes vaginalis.
- Congenital inguinal hernia: also due to failure of obliteration of the connection between the peritoneum & the processes vaginalis.
Development of the ovary
Steps of development
- In female embryos with an XX sex chromosome complement and no Y chromosome, primitive sex cords dissociate into irregular cell clusters, These clusters, containing groups of primitive germ cells, occupy the medullary part of the ovary (medullary cords), Later they disappear and are replaced by a vascular stroma that forms the ovarian medulla.
- The surface epithelium continues to proliferate & gives rise to 2nd generation of cords (cortical cords).
As the cortical cords increase in size, the primordial germ cells are incorporated into them, The cortical cords are split into isolated cell clusters (primordial follicles) each consists of oogonia (developed from primordial germ cells) surrounded by follicular cells.
Descent of the ovary
The ovary is found in the abdominal cavity, so the descent of the ovary to the pelvic cavity occurs through contraction of the gubernaculum. The gubernaculum is attached to the uterus. This leads to the division of the gubernaculum into 2 parts. One part extends from the uterus to the inguinal canal called the round ligament of the uterus. The other part extends from the ovary to the uterus called the ovarian ligament.
Abnormalities
Ectopic ovary: the ovary may be found in the inguinal canal or in the labia majora.
Development of genital ducts
A. Indifferent stage
Initially, both male and female embryos have two pairs of genital ducts: mesonephric (Wolffian) ducts and paramesonephric (müllerian) ducts.
B. Mesonephric duct (Wolffian duct)
The mesonephros and mesonephric ducts are derived from intermediate mesoderm from upper thoracic to upper lumbar (L3) segments (refer to the urinary system development).
The mesonephric tubules
In males, the mesonephric tubules will persist as a few excretory tubules, the epigenital tubules which establish contact with cords of the rete testis and finally form the efferent ductules of the testis, Excretory tubules along the caudal pole of the testis, the paragenital tubules, do not join the cords of the rete testis, Their vestiges are collectively known as the paradidymis, In females, the mesonephric tubules degenerate except epoophron and paroophron.
The mesonephric duct
Except for the most cranial portion, the appendix epididymis, the mesonephric ducts persist and form the main genital ducts in males (body and tail of epididymis, vas deferens, seminal vesicle and ejaculatory duct), In females, the mesonephric duct degenerates except for the duct of epoophron and Gartner’s duct.
C) Paramesonephric duct (Mullerian duct)
In female:
Origin: The paramesonepheric duct arises as a longitudinal epithelial invagination of the epithelium lateral to the mesonepheric duct. This duct extends caudally to protrude in the dorsal wall of the urogenital sinus forming the Mullerian Tubercle. During the descent of the para-mesonepheric duct; it shifts from the lateral side of mesonepheric duct to the medial side. The 2 paramesonepheric ducts meet & fuse the septum between them disappeared forming a single canal called the uterovaginal canal.
Development of the uterus
It developed from the paramesonepheric ducts. It is divided into 3 parts:
- The cranial vertical part (future uterine tubes).
- Middle horizontal part (future horns of the uterus).
- Caudal vertical part called uterovaginal canal (future body of the uterus, cervix & upper 3/5 of the vagina).
Development of the vagina
It develops from:
- The proliferation of the caudal end of the uterovaginal canal, leads to the formation of the vaginal cord.
- The proliferation of the Mullerian tubercle (the posterior wall of the urogenital sinus. leads to the formation of sinovaginal bulb. Fusion of the vaginal cord and sinovaginal bulb forms a vaginal plate. Canalization of the plat leads to the formation of the lower 2/5 of the vagina. This canalization is incomplete at the caudal end of the vaginal plat leads to the formation of the hymen.
- The definitive urogenital sinus gives the vestibule of the vagina.
- The upper 3/5 of the vagina originated from the caudal part of the uterovaginal canal.
Fate of Mullerian duct in male
- Its upper part gives the appendix of the testis.
- Its lower part gives the prostatic utricle.
Congenital anomilies of the female genital ducts
A)- Anomalies due to failure of fusion of the 2 paramesonephric ducts:
- Double uterus & double vagina: due to complete failure of fusion of the 2 ducts.
- Double uterus, double cervix & single vagina: due to partial failure of fusion of the 2 ducts.
- Double uterus, single cervix & single vagina: due to partial failure of fusion of the 2 ducts.
- Bipartite uterus: a small septum remains in the upper part of the uterine cavity.
- Arcuate uterus: fundus is depressed due to a minor degree of imperfect fusion of the 2 ducts.
B)- Anomalies due to complete or partial atresia of paramesonephric ducts:
- Bicornuate uterus with a rudimentary horn: one paramesonephric duct retard in growth.
- Atresia of the cervix: due to failure of canalization of the cervical canal.
- Atresia of the vagina: due to failure of canalization of the vaginal plate.
- Imperforate hymen: due to failure of perforation of the inferior end of the vaginal plate.
Development of external genitalia
I. Indifferent Genitalia
This stage is common in male and female, The proliferation of mesenchyme on each side of the cloacal membrane form cloacal folds, Three structures are then formed:
- Genital tubercle (Phallus) (formed by fusion of the cranial end of the cloacal folds).
- Urethral (Urogenital folds) (formed by the anterior part of the cloacal folds on each side of the cloacal membrane – The posterior part of the cloacal folds is called anal folds).
- Lateral genital swellings (6th week) (another two swellings lateral to the urethral folds).
– At the same time, the cloacal membrane is subdivided into a urogenital membrane and an anal membrane.
II. Different Genitalia
A. External genitalia in male:
Cause: Androgens secreted by fetal testis.
The three structures around the cloacal membrane will give the following:
- Genital tubercle (phallus): It elongates and enlarges to form the penis.
- Urethral folds: As the genital tubercle (phallus) elongates to form the penis, it pulls the phallic part of the urogenital sinus and urethral folds forwards. The urethral folds form the urethral groove which is covered by the endoderm (derived from the phallic part of the urogenital sinus) called the urethral plate. The urethral groove fuses (closes) on the ventral aspect of the penis to share in the formation of the penile urethra.
- Lateral genital swellings: They fuse with each other to form the scrotum which is formed of two halves separated by the scrotal septum. The urogenital membrane ruptures and the definitive urogenital sinus becomes continuous with the urethra.
Congenital anomalies
- Hypospadius.
- Epispadius.
- Megalopenis: Abnormally large penis due to abnormal dilatation of penile urethra.
- Double penis (very rare): It is due to partial subdivision of the penis due to incomplete fusion of the two sides of the genital tubercle.
- Micropenis: Cause: Insufficient androgen stimulation for growth of the external genitalia. It occurs in primary hypogonadism or hypothalamic or pituitary dysfunction.
- Ectopiavesica.
B. External genitalia in female
Cause: Estrogens stimulate the development of the external genitalia of female. The three structures around the cloacal membrane will give the following:
- Genital tubercle (phallus): It forms the clitoris.
- Urethral folds: They don’t fuse and form labia minora.
- Lateral genital swellings: They don’t fuse and enlarge to form labia majora. The urogenital membrane ruptures and the definitive urogenital sinus forms the vestibule.
Congenital anomalies
- Labial fusion: It is due to the fusion of the two labia majora to a great extent leading to the formation of just a small opening for the passage of urine from the urethra.
- Imperforate hymen: It arises as solid endodermal outgrowths from the definitive urogenital sinus (corresponds to bulbourethral glands in male).
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Female reproductive system organs, functions, anatomy and Histological structure of the uterus
Ovary function, location, anatomy, structure, Oogenesis, and maturation of primary oocyte
Fallopian tubes function, location, anatomy and Histological structure of vagina
Ovarian hormones, Menopause, Functions of estrogen and progesterone in pregnancy