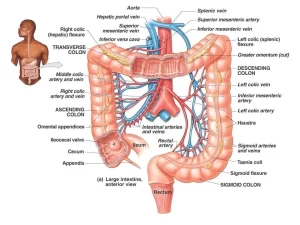
Histological structure of large intestine, vermiform appendix and alimentary canal
The large intestine is about 1.5 metres long and has an average diameter of about 6 cm. The functions of the large intestine are a recovery of water and electrolytes, formation and storage of faeces and fermentation of some of the indigestible food matter by bacteria.
Histological structure of the large intestine
The large intestine includes several anatomical segments; the caecum, the colons (ascending, transverse, descending, and sigmoid), and also the rectum. Histologically. they share common general features.
Histological organization of the large intestine
Mucosa
The colonic mucosa is characterized by:
- The surface epithelium is smooth, with no villi.
- Its lamina propria contains a large number of tubular intestinal glands (crypts of Lieberkühn).
- The colonic crypts of Lieberkühn extend throughout the full thickness of mucosa, perpendicular to the muscularis mucosae with their openings on the luminal surface.
- They are straight, parallel to each other and densely packed together with minimal connective tissue lamina propria in between.
The colonic surface epithelium and the colonic crypts are lined by the following types of cells:
- The columnar absorptive cells: they have short microvilli on their luminal surface for absorption of water from the residuals of the digested food.
- Goblet cells: present in a huge number.
- Enteroendocrine cells; are present in a small number, such as EC cells secreting serotonin and L cells secreting enteroglucagon.
- Stem cells: located at the bases of the crypts.
The lamina propria is formed of loose connective tissue, occupied by numerous intestinal glands. It is rich in lymphoid nodules located at the bases of the crypts. The muscularis mucosae underlying the bottom of the crypts and is formed of inner circular and outer longitudinal layers of smooth muscle fibers.
Submucosa
Musculosa
It is formed of a complete inner circular layer of smooth muscle fibers. The outer longitudinal layer is incomplete and condensed into three bands of longitudinal smooth muscle fibers, called the teniae coli. The teniae coli are seen grossly on the outer surface of the colon, giving it the characteristic sacculations (haustration).
Serosa
It is formed of loose connective tissue covered by the mesothelium. Small peritoneal projections filled with adipose tissue, the appendices epiploicae are seen protruding on the outer surface of the colon at the sites of the deficient longitudinal muscle fibers.
Histological structure of the vermiform appendix
The appendix is a blind-ended narrow evagination of the caecum. It is a significant part of the mucosa-associated lymphoid tissue (MALT).
Histological organization of a section in the appendix:
It has a narrow, irregular lumen that may be filled with dead cells, blood, and other debris.
Mucosa
It is similar to that of large intestine; however the crypts of Lieberkühn are characterized by the following: They are formed of a few numbers of widely-separated, short tubular glands. They have no digestive or absorptive functions in human. They are lined by:
- Simple columnar cells.
- Goblet cells.
- Many enteroendocrine cells particularly EC cells.
The lamina propria is filled with loose (scattered lymphocytes) and dense lymphoid tissue (lymphoid nodules) occupying the spaces between the crypts and extending around the whole circumference of the appendix. The muscularis mucosae is not well-defined and is usually interrupted by the lymphoid tissue that penetrates into the submucosa.
Submucosa
It is a narrow layer that is also filled with lymphoid tissue.
Musculosa:
It is formed of inner circular and complete outer longitudinal smooth muscle layers.
Serosa:
Junctional sites between the different parts of the alimentary canal
Three main junctional sites along the alimentary canal are of histological interest. They are studied by longitudinal sections at the site of the junction, thus demonstrating evident variations in the structure of their wall as passing down from a part to the successive one. These junctions are:
- The esophago-gastric junction.
- The pyloro-duodenal junction.
- The recto-anal junction.
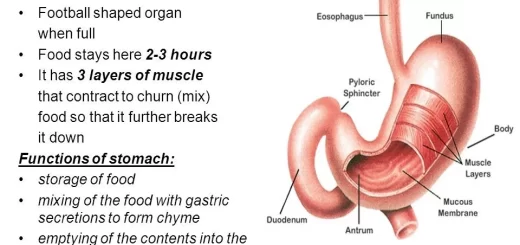
The esophagogastric junction
Mucosa:
The surface epithelium changes abruptly from the non-keratinized stratified squamous, lining the esophageal end, to the simple columnar epithelium of the cardiac end of the stomach. The columnar epithelium of the stomach is interrupted by gastric pits characteristic of the cardiac region. The lamina propria at the esophageal end, containing the mucosal esophageal glands, becomes wider and shows the branched tubular cardiac glands.
Submucosa
The submucosal esophageal glands may continue for a variable distance into the submucosa of the cardia.
Musculosa
It becomes thicker at the cardiac region with additional inner oblique smooth muscle fibers.
Serosa:
The abdominal end of the esophagus has already acquired a mesothelial covering continuous with that of the stomach.
The pyloro-duodenal junction
Mucosa
The surface epithelium undergoes gradual changes; the columnar surface mucous cells acquire a brush border and become absorptive cells. The epithelium starts to project into the lumen forming the typical villi of the first part of the duodenum. In the lamina propria, the intestinal crypts of Lieberkühn replace the pyloric glands. Scattered goblet cells appear in between the columnar cells covering the villi and lining the crypts.
Submucosa
Large numbers of mucous acini of Brunner’s glands appear.
Musculosa
The thick inner circular muscle layer that forms the pyloric sphincter becomes thinner towards the duodenum, as thick as the outer longitudinal muscle layer.
Serosa
Both the pylorus and duodenum are covered by the visceral layer of the peritoneum.
The recto-anal junction
Mucosa & Submucosa:
The rectal mucosa is typical to that of the large intestine except that the crypts of Lieberkühn become shorter and gradually disappear. The upper part of the anal canal shows longitudinal mucosal folds known as the anal columns of Morgagni. The distal ends of the anal columns are connected by short transverse mucosal folds known as the anal valves, marking the pectinate line at the muco-cutaneous junction.
The surface epithelium gradually changes from simple columnar epithelium with goblet cells into stratified columnar epithelium on the anal columns. At the level of the anal valves, the epithelium further changes into the non-keratinized stratified squamous epithelium.
About 1cm above the anal orifice (at the level of the white line), the epithelium finally changes into the epidermis, keratinized stratified squamous epithelium continuous with that of the peri-anal skin. This part is covered by typical thin skin with hair follicles, sebaceous glands and the circumanal apocrine sweat glands.
At the level of the anal columns, the muscularis mucosae fades out and the lamina propria blends with the submucosa of the anal canal. The submucosa in this area contains the internal rectal venous plexus and is rich in diffuse lymphoid tissue. The connective tissue dermis under the anal orifice contains another venous plexus. the external rectal venous plexus.
Musculosa
The inner circular smooth muscle layer is thickened to form the internal anal sphincter. Distal and outer to the internal anal sphincter, circumferential bundles of skeletal muscles form the external anal sphincter.
Adventitia
The adventitia of the rectum is continuous with the connective tissue dermis of the peri-anal skin.
Clinical hint: the venous plexuses of the recto-anal junction might become dilated and congested leading to the development of piles (hemorrhoids).
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Histological structure of the small intestine, Mucosa, Submucosa and Intestinal glands
Large Intestine function, parts, length, anatomy & Relations of the rectum
Pancreatic secretion composition, regulation, function, Differences between jejunum & ileum
Bile salts & gall bladder function, Factors affecting gall bladder evacuation (Cholagouges)