Blood groups, Rh blood groups, Erythroblastosis fetalis and Importance of Rh factor
Hundreds of different antigens have been found on the surfaces of human blood red cells. Most of these are weak and are mainly of importance in genetic studies, however, two particular groups of antigens are more likely than others to cause blood transfusion reactions. These are the so-called O-A-B system and Rh system.
O-A-B blood groups
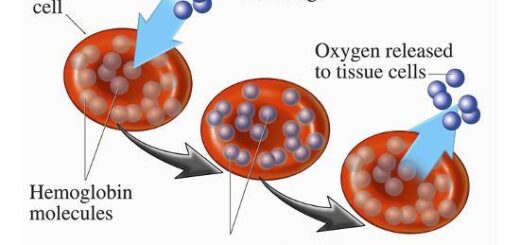
Two related antigens (type A and type B) occur on the surfaces of the red blood cells in a large proportion of the population. Strong antibodies that react specifically with either type A or type B antigens almost always occur in the plasmas of persons who do not have the antigens on their red blood cells. These antibodies can bind with the red cell antigens to cause agglutination (clumping together) and haemolysis of red blood cells.
Therefore, type A and type B antigens are called agglutinogens, and the plasma antibodies are called agglutinins. Individuals are normally classified into 4 major O-A-B types depending on the presence or absence of the two agglutinogens.
The relative frequencies of different blood types: Blood type O is 46%, Blood type A is 42%, Blood type B is 9%, Blood type AB is 3%, It is obvious from the percentages that the O & A genes occur frequently whereas the B-gene is infrequent.
Dangerous hemolytic transfusion reactions occur when blood is transfused into an individual with an incompatible blood type, that is, an individual who has agglutinins against the red cells in the transfused blood. The plasma in the transfusion is usually so diluted in the recipient that it rarely causes agglutination. However, when the recipient’s plasma has agglutinins against the donor’s red cells, the cells agglutinate and hemolyze.
Rh blood groups
Rh is a system composed primarily of the C, D, and E antigens, although it actually contains many more. D is by far the most antigenic component, and the term Rh-positive is generally used to the individual that has agglutinogen D, whereas those persons who do not have type D-antigen are said to be Rh-negative. Approximately 85% of all white races are Rh-positive and 15% are Rh-negative, In American blacks, the percentage of Rh-positive is 95, whereas in African blacks it is about 100%.
Thus, persons with type AB Rh-positive blood are “universal recipients” because they have no circulating agglutinins and they can take blood from any type without developing transfusion reactions. Type O Rh-negative individuals are universal donors because there are no agglutinogens in their blood and thus can be given to anyone without producing transfusion reactions due to O-A-B or Rh incompatibility.
Importance of the Rh factor (Rhesus factor)
Before blood transfusion: When an Rh-negative person is injected with red blood cells containing Rh factor, anti-Rh agglutinins develop very slowly and cause an immediate reaction. The maximum concentration of agglutinins occurs 2-4 months later. On subsequent transfusion of Rh-positive blood into the same person, a very high amount of anti-Rh agglutinins develops and severe transfusion reactions will occur.
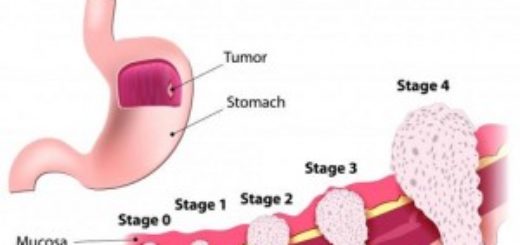
Haemolytic disease of the newborn (Erythroblastosis fetalis): When the mother is Rh-negative and father is Rh-positive, if the fetus has inherited the Rh-positive antigen from the father, eythroblastosis fetalis may result. Small amounts or fetal blood may leak into the maternal circulation at the time of delivery.
Some mothers develop significant amounts of anti-Rh agglutinins after labour. The first baby is usually born normal. During the next pregnancy, the mother anti Rh-agglutinins diffuse through the placenta into the fetus and can cause agglutination and haemolysis of the fetal red blood cells. If the haemolysis is severe, the infant may die in utero or may develop erythroblastosis fetalis.
The main manifestations of erythroblastosis fetalis are:
- Anemia.
- Severe jaundice.
- Many immature red blood cells (erythroblasts) in the fetal blood.
- Kernicterus: A neurologic disease may develop due to the deposition of bile pigments in some centers (motor areas) causing their damage. Bile pigments do not enter the brain in the adult, but in the fetus and newborns, the blood-brain barrier is not yet developed.
Prevention of erythroblastosis fetalis
It is possible to prevent it from occurring the first time by the administration of a single dose of anti-Rh antibodies in the form of Rh immunoglobulins after labour (within 72 hours postpartum period). Such passive immunization prevents active antibody formation by the mother. This has to be done every pregnancy, every abortion or any cause of fetomaternal haemorrhage as severe trauma.
Anemias causes, symptoms, features, diagnosis & Types of Polycythemia
Functions and sources of Folic acid, Cobalamin (vitamin B12) & Vitamin K
Factors that help iron absorption, Daily iron requirements & Abnormal iron levels