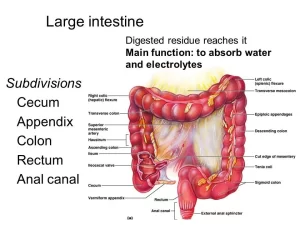
Large Intestine function, parts, length, anatomy and Relations of the rectum
The large intestine reabsorbs the water and mineral ions such as sodium and chloride, It can form and temporary store faeces, It maintains over 500 species of bacteria, It includes the colon, rectum, and anus, long tube that continues from the small intestine as food nears the end of its journey through your digestive system. It turns food waste into a stool and passes it from the body when you poop.
Anatomy of Large Intestine
Length: is about 1.5 meters.
Parts:
- Caecum and appendix.
- Colons (ascending, transverse, descending, and pelvic with 2 colic flexures in between).
- Flexures (right and left colic flexures).
- Rectum.
- Anal Canal.
The Small and Large intestine:
the large intestine shows 3 features that are absent in the small intestine.
- Tenia Coli: are the longitudinal outer muscle layer which is represented by 3 bands, They are not found in the appendix and rectum.
- Sacculations: (haustrations) this is due to the length of tenia coli is shorter than the length of the large intestine.
- Appendices Epiploicae: small sacs of peritoneum-covered fat hanging from the surface of the colon.
Large Intestine:
- Tenia coli: Present.
- Sacculations: Present.
- Appendices epiploicae: Present.
Small intestine:
- Tenia coli: Absent.
- Sacculations: Absent.
- Appendices epiploicae: Absent.
Caecum
It is a mobile blind sac at the beginning of the large intestine.
Position: It occupies the right iliac fossa and is completely covered with the peritoneum.
Relations:
- Anteriorly: anterior abdominal wall, greater omentum, and coils of the small intestine.
- Posteriorly: 2 Muscles: Psoas major and iliacus. 2 Nerves: Femoral and lateral cutaneous nerve of the thigh.
Communications of the caecum
- Terminal ileum: opens into the posteromedial aspect of the caecum ileocecal orifice, guarded by the ileocecal valve.
- Appendix: opens into the posteromedial aspect, inferior to the ileocecal opening.
- Ascending colon: continuous upwards with it.
Blood supply of caecum
- Arterial supply: anterior and posterior caecal arteries from the ileocolic artery which is a branch from the superior mesenteric artery.
- Venous drainage: into the superior mesenteric vein then into the portal vein.
Vermiform appendix
It is a worm-like tube, about 10 cm long, that opens by its base into a posteromedial aspect of the caecum below the terminal ileum. It has a mesentery known as mesoappendix which is a triangular peritoneal fold, containing the appendicular artery in its free border.
Positions of the Appendix
- Retrocecal (65%).
- Pelvic (30%).
- Subcecal (3%).
- Pre or post-ileal (2%).
Blood supply of the appendix
- Arterial supply: appendicular artery from the posterior caecal artery from the ileocolic artery.
- Venous drainage: into a superior mesenteric vein.
Surface anatomy of the base of the appendix
(McBurney’s point): It is represented by a point at the junction between the lateral 1/3 and medial 2/3 of a line drawn from the anterior superior Iliac spine to the umbilicus.
Clinical note: Inflammation of the appendix (appendicitis) causing ill-defined colicky pain, felt in the umbilical region because, the appendix is supplied with sympathetic fibers from the 10th thoracic spinal cord segment, and the 10th thoracic somatic nerve supplies the skin of the umbilical region.
Ascending colon
It begins as a continuation of the cecum and ends just below the liver, where it continues with the transverse colon at the right colic (hepatic) flexure. The peritoneal covering is covered by the peritoneum anteriorly and on each side.
Blood supply:
Arterial supply: From superior mesenteric artery
- lleocolic artery
- Right Colic artery
Venous drainage: It drains into veins corresponding to the arterial supply.
Transverse colon
It runs from the right colic (hepatic) flexure across the abdomen to the left colic (splenic) flexure, It is completely covered with peritoneum which forms transverse mesocolon and it is freely mobile.
Transverse mesocolon
The transverse colon is suspended from the posterior abdominal wall by its transverse mesocolon which is attached to the anterior border of the pancreas.
Contents of the transverse mesocolon
- Transverse colon.
- Middle colic artery.
- Extra-peritoneal fat.
- Sympathetic nerves.
Blood supply:
Arterial supply:
- Right 2/3 by right and middle colic arteries of the superior mesenteric artery.
- Left 1/3 by the ascending branch of the left colic artery from the inferior mesenteric artery.
Venous drainage: It drains into the veins corresponding to the arterial supply.
Descending colon
It runs from the left colic (splenic) flexure and descends till the pelvic brim to continue as the sigmoid (pelvic) colon. Peritoneal coverings are covered by the peritoneum anteriorly and on each side.
The left colic flexure is higher than the right flexure and attached to the diaphragm by a peritoneal fold called phrenico-colic ligament which prevents vertical descent of the spleen into the left iliac fossa in case of splenomegaly.
The right colic flexure (hepatic) is related anteriorly to the livers and posteriorly to the kidney. The left colic flexure (splenic) is related laterally and superiorly to the spleen and posteriorly to the diaphragm.
Pelvic (sigmoid) colon
The pelvic colon begins at the left side of the pelvic brim, It ends at the 3rd sacral piece where the rectum begins, It describes an S-shaped course, and it is completely covered with peritoneum and suspended by the sigmoid mesocolon.
Blood supply
Arterial supply: sigmoid branches of the inferior mesenteric artery.
Venous drainage: It drains its venous blood into the veins corresponding to the arterial supply.
Sigmoid mesocolon: is a peritoneal fold that is attached to the posterior pelvic wall by an inverted V-shaped root.
- Sigmoid mesocolon (v-shaped) has an apex and two limbs:
- The apex of the mesocolon lies anterior to the left ureter at the point of bifurcation of the left common iliac artery.
- Mediallimb: descends in front of the sacrum and ends opposite the 3rd sacral piece.
- Lateral limb: extends along the left side of pelvic brim along the left external iliac vessels.
Contents of the sigmoid mesocolon
- Sigmoid colon in the free border.
- Sigmoid vessels in the lateral limb.
- Superior rectal vessels in the martial limb.
Rectum
It begins at the 3rd sacral piece as a continuation of the sigmoid colon, It follows the concavity of the sacrum & coccyx (sacral flexure). It ends at the recto-anal junction, about 1 inch in front and below the tip of the coccyx by bending posteriorly (perineal flexure). Its lower part is dilated and is called the “ampulla of the rectum”.
Peritoneal covering
- Upper 1/3rd front and sides are covered by peritoneum.
- The Middle 1/3rd front is only covered by the peritoneum.
- The lower 1/3rd has No peritoneal covering.
Lateral Flexures & Mucosal folds (valves)
1. Lateral flexures:
- Upper flexure: Concave to the left side.
- Middle flexure: Concave to the right side.
- Lower flexure: Concave to the left side.
2. Antero-posterior flexures:
- Sacral flexure: It is concave forwards (following the concavity of the sacrum).
- Perineal flexure: It is convex forwards and lies at the recto-anal junction. The mucous membrane show 3 transverse folds. These support faecal matter.
Relations of the rectum
In males
Anterior:
- The recto-vesical pouch containing coils of ileum and sigmoid colon.
- The base of the urinary bladder.
- Ampulla of vas deferens.
- Seminal vesicles.
- Prostate.
- The terminal part of the ureter.
Posterior:
- Muscles: Piriformis, LevatorAni, Coccygeus.
- Bones: Sacrum, Coccyx
- Vessels: Superior Rectal Artery, and Median Sacral Artery.
- Nerves: Sympathetic Trunks, Lower 3 Sacral Nerves, and Coccygeal Nerve.
Laterally: Levator Ani, Coccygeus, Pararectal Fossa.
In females
Anterior:
- Recto-uterine pouch, coils of ileum, and sigmoid colon.
- The posterior wall of the vagina.
Posterior:
- Muscles: Piriformis, LevatorAni, Coccygeus.
- Bones: Sacrum, Coccyx
- Vessels: Superior Rectal Artery, and Median Sacral Artery.
- Nerves: Sympathetic Trunks, Lower 3 Sacral Nerves, and Coccygeal Nerve.
Laterally: Levator Ani, Coccygeus, Pararectal Fossa.
Blood supply of the rectum
Arterial supply
- Superior rectal artery: It is the continuation of the inferior mesenteric artery, It supplies the rectum and upper half of the anal canal.
- Middle rectal artery: It arises from the anterior division of the internal iliac artery.
- Inferior rectal artery: It arises from the internal pudendal artery.
Venous drainage
- The superior rectal vein continues up as the inferior mesenteric vein which drains into the splenic vein. (Portal circulation).
- Middle rectal vein: Drains into the internal iliac vein (Systemic circulation).
- Inferior rectal vein: Drains into the internal pudendal vein (Systemic circulation).
Superior, middle, and inferior rectal veins anastomose with each other in the submucosa of the rectum and anal canal. Hemorrhoids (piles) is the dilation of the veins at the site of anastomosis.
Lymph drainage
- Upper half drains to the para rectal L.Ns which drain to the inferior mesenteric LNs.
- The lower half drains to the internal iliac lymph nodes.
Anal canal
- Beginning: It begins one inch below and anterior to the tip of the coccyx at the rectoanal junction.
- Course: It runs downwards and backwards.
Mucocutaneous lining of anal canal:
The upper part of the anal canal is lined by mucous membrane while the lower part is lined by skin. The mucous membrane lining the upper part is thrown into longitudinal folds called anal columns. The lower ends of anal columns are connected by crescentic folds of mucous membranes called anal valves.
The line of the anal valves is called the pectinate line. According is about 23 mm above the anal orifice. It marks the site of the anal membrane. The white line is a pale bluish pink line that lies 15 mm below the pectineal line.
Termination: It ends at the anus.
Relations:
- Laterally: Ischioanal fossae.
- Posteriorly: Anococcygeal raphe between it and the tip of the coccyx.
- Anteriorly: Perineal body between it and the bulb of the penis in males, The perineal body between it and the vagina in females.
Blood supply, nerve supply, and lymph drainage of the anal canal:
Upper part (half):
- Blood supply: It is supplied by the superior rectal artery, It is drained by the superior rectal vein (portal circulation).
- Nerve supply: Above the pectinate line by autonomic nerve fibers. Insensitive to pain 8 touch.
- Lymphatic drainage: Above the pectinate line into internal iliac LNs.
Lower part (half):
- Blood supply: It is supplied by: Middle rectal artery of the internal iliac artery, and the Inferior rectal artery of the internal pudendal artery. The corresponding veins drain into the internal iliac vein (systemic circulation.)
- Nerve supply: Below the pectinate line by the inferior rectal nerve (Sensitive to pain, touch).
- Lymphatic drainage: Below the pectinate line into superficial inguinal LNs.
Anal sphincters
Internal anal sphincter: It is the thickened inner involuntary circular muscle layer of the anal canal, It surrounds the upper 3/4th of the anal canal, extending from the anorectal junction till the white line (Hilton’s line).
Nerve supply: autonomic
External anal sphincter: Striated voluntary muscle fibers, Surrounds the whole length of the anal canal outside the internal anal sphincter.
Parts:
- Subcutaneous Part: Surrounds the anus just under the perianal skin, and is attached to the perineal body and anococcygeal raphe.
- Superficial Part: Surrounds the lower part of the internal sphincter above the subcutaneous part. It takes origin from the anococcygeal body and the last piece of the coccyx.
- Deep part: It encircles the upper part of the anal canal and has no bony attachments.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Pancreatic secretion composition, regulation, function, Differences between jejunum & ileum
Small intestine function, anatomy, parts, Arterial supply of the duodenum, midgut & hindgut
Stomach parts, function, curvatures, orifices, peritoneal connections & Venous drainage of Stomach