Bile salts and gall bladder function, Factors affecting gall bladder evacuation (Cholagouges)
The liver cells synthesize about 0.2-0.4g of bile salts per day. They are sodium and potassium salts of bile acids (glycocholic, and taurocholic acids). The bile acids are synthesized from cholesterol. The conjugation of cholic acid with the amino acid glycine forms glycocholic acid, and with taurine forms taurocholic acid, Taurine is a derivative of the amino acid cysteine.
Bile salts
Normally the liver manufactures a minute amount of bile salts because about 95% of the already formed bile salts are reabsorbed again from the small intestine into the portal blood and re-secreted by the liver with bile (entero-hepatic circulation of bile salts).
The remaining 5-10% of the bile salts enter the colon and are converted to the salts of deoxycholic acid and lithocholic acid, Lithocholate is relatively insoluble and is mostly excreted in the stools, However, deoxycholate is absorbed.
Functions of bile salts
1. Digestion of fat: Bile salts have no direct digestive effects, but help fat digestion by their emulsifying or detergent function, Emulsification decreases the surface tension of the particles and allows a good surface area to be exposed to the action of pancreatic lipase, Bile salts also activate lipase enzymes.
2- Absorption of fat: Bile salts tend to form cylindrical water-soluble disks called “micelles”, The micelle contains fatty acids, monoglycerides, phospholipids, and cholesterol, Thus, it solubilizes the lipids and provides a mechanism for their transport to the enterocytes, The micelles move down their concentration gradient through the brush border of the intestinal mucosal cells, where they are absorbed.
Then, the lipids diffuse out of the micelles, and the absorbed bile salts are transported back to the liver in the portal vein and re-excreted in the bile (enterohepatic circulation), Bile salts can dissolve the insoluble fatty acids in water, thus the fatty acids formed are removed from the medium and new molecules of neutral fat are exposed to the action of pancreatic lipase.
Bile salts facilitate the absorption of fat-soluble vitamins (D, E, K) and carotenes, Absorption of fatty acids also helps indirectly the absorption of calcium and iron by preventing their precipitation in an insoluble form.
3. Solvent action: Because bile salts prevent the precipitation of cholesterol and fatty acids by keeping them in solution, they guard against gall stones formation.
4. Choleretic function: Bile salts are the best choleretics (stimulants for bile secretion by liver cells), Absorption of any amount of the secreted bile salts in the intestinal mucosa, passes via the portal circulation to the liver, leading to stimulation of bile secretion
5. Stimulation of peristalsis: Bile salts stimulate the motility of the intestine and colon and prevent constipation.
6. Ant-putrefactive action: Bile salts have no direct antiseptic effect, but they prevent putrefaction by absorption of fats, In their absence, undigested fat covers the protein particles and hinders their digestion, The undigested protein particles in the large intestine are attacked by bacteria leading to putrefaction.
Regulation of bile secretion
Hepatic cells continuously secrete bile under low biliary pressure, Any factor which stimulates bile secretion is called “choleretic”. This is controlled by:
I. Humoral mechanisms
- Bile salts: They are the most powerful choleretics known, Bile salts are evaluated with bile from the liver to the intestine. After performing their function, 95% of them are absorbed from the terminal ileum by an active transport mechanism. On reaching the liver they stimulate it to secrete bile, which is deficient in bile pigments (enterohepatic circulation of bile salts).
- Secretin: In addition to its stimulant effect on pancreatic secretion it stimulates the bile secretion by increasing its water and bicarbonate content, so it is called “hydrocholeretic”.
II. Nervous factors
The parasympathetic supply carries mainly stimulatory secretory fibers, so its stimulation it increases bile secretion, The sympathetic supply exerts its effect on bile secretion through vasoconstriction which decreases the blood flow and in turn decreases bile secretion.
III. Blood flow
Increased portal blood during digestion increases bile secretion, but when the liver is markedly congested bile secretion stops due to an increase in the intrahepatic vascular pressure.
Functions of the gall bladder
1- Storage of bile
Bile flows into the duodenum only after ingestion of food, In between the meals, the sphincter of Oddi is closed and bile flows back to the cystic duct to be stored in the gall bladder.
2- Concentration and acidification of bile
The total daily secretion of bile is about 500 ml, while the maximum volume of the gall bladder is only 40-70 ml. Nevertheless, as much as 12 hours of bile secretion can be stored because its water, sodium chloride, and most other small molecular weight electrolytes are absorbed by the gall bladder mucosa.
The other bile constituents are concentrated, Bile can be concentrated up to 10 or 12 times, Acidification is done by absorption of its NaHCO3 content, which prevents the precipitation of insoluble calcium salts, and the formation of gall stones, Also, acidity has a bactericidal effect.
3- Secretion of white bile
Gall bladder and bile duct mucosa secrete mucoid-like material which protects them from any irritant chemical products.
4- Buffering of biliary pressure
The gall bladder equalizes the pressure in the biliary system, By storing bile, it prevents any increase in pressure in biliary passages, This enables the liver to secrete because hepatic cells cannot secrete against high pressure.
5- Evacuation of bile when needed
Hepatic cells secrete bile at low pressure, about 7 cm H2O. The tonic contraction of the sphincter of Oddi is equivalent to 30 cm H20 when it is closed (in between meals). After ingestion of food, there is a partial relaxation of the sphincter with a tone of about 10 cm H20, synchronous with contraction of the gallbladder with a pressure equal to 20 cm H20, In this case, the bile flows from the gall bladder together with the fresh bile coming from the liver to the duodenum.
Gall bladder evacuants are called “cholagogues” to differentiate between them and those agents which stimulate bile secretion from the liver which are called “choleretics”
Factors affecting gall bladder evacuation (Cholagouges):
1. Hormonal factor: Cholecystokinin (CCK). This local hormone is secreted when fatty acids or amino acids reach the duodenum. It circulates in the blood and passes to the gall bladder via its blood supply and leads to contraction of the gall bladder wall and evacuation of its contents into the duodenum.
2. Nervous factors. The nervous factors play a minor role in bile evacuation. The vagus nerve is motor to the wall of the gall bladder and inhibitory to the sphincter of Oddi. After parasympathetic stimulation, the gall bladder contracts, and bile is collected into the bile ducts and flows into the duodenum with the aid of the relaxation phase of the peristaltic wave travelling along it. Sympathetic stimulation inhibits the gall bladder wall, but contracts the sphincter.
It can be concluded that the hormonal factor is the most important in bile secretion and evacuation.
You can download Science online application on google Play from this link: Science online Apps on Google Play
Histological structure of gallbladder & Pancreas, Functions of the liver & Composition of bile
Portal Venous System, Histological structure of Liver, portal vein and its tributaries
Histology of pancreas, Structure of islets of Langerhans, Insulin function & Metabolism
Small intestine function, anatomy, parts, Arterial supply of the duodenum, midgut & hindgut
Pancreas function, anatomy, parts, relations, ducts & blood supply
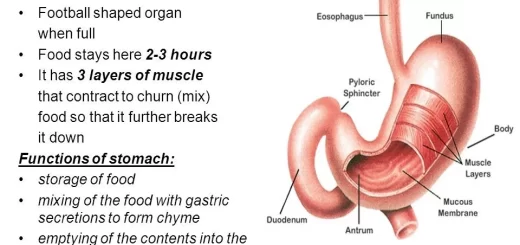
Stomach parts, function, curvatures, orifices, peritoneal connections & Venous drainage of Stomach