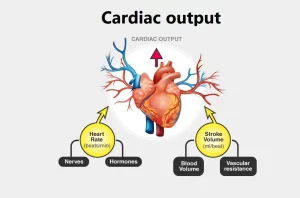
Factors affecting cardiac output, Stroke volume, Heart rate and blood pressure
The stroke volume (SV) is the amount of blood pumped out from each ventricle per beat. It is about 70-90 ml in a resting man of average size in the supine position. It equals the end-diastolic volume minus the end-systolic volume. End diastolic volume is the volume of blood in each ventricle at the end of the diastole. It equals 130 ml; it is affected by the venous return.
The cardiac output
The cardiac output is the amount of blood pumped out from each ventricle per minute. In a resting, supine man, it averages about 5.5 L/min (80 mL x 70 beats/ min). The cardiac index is the cardiac output/minute/square meter of body surface area. It averages about 3.2 L/min/m2.
Cardiac output (CO) is a crucial metric for assessing cardiovascular health as it reflects the body’s ability to deliver oxygen and nutrients to tissues. CO is calculated by multiplying stroke volume (SV), the amount of blood ejected with each heartbeat, by heart rate (HR).
End systolic volume is the volume of blood in each ventricle at the end of the systole. It is about 50 ml; it is affected by arterial blood pressure & cardiac contractility (increased arterial blood pressure and decreased cardiac contractility decrease stroke volume & increase end-systolic volume).
The ejection fraction is the percentage of the end-diastolic volume that is ejected with each stroke. It is about 60-65 %. The ejection fraction is a valuable index of ventricular function.
Factors determining the Cardiac Output
The cardiac output = heart rate X stroke volume
Changes in cardiac output that are called for by physiologic conditions can be produced by changes in heart rate or stroke volume or both. The heart rate has a direct effect on the cardiac output, if increases, the cardiac output increase. However, if the heart rate increases so much to the extent that it shortens the diastolic time.
The cardiac output may decrease rather than increase. This is explained on the bases that the normal diastolic time in a person with an average heart rate of 70 beats/min is 0.5 sec. During this period, coronary and heart filling take place. Too much increase in heart rate shortens the diastolic time and decreases the end-diastolic volume, the force of contraction, and stroke volume. This results in decreased cardiac output.
Stroke volume: When the stroke volume is increased, it would increase the cardiac output, provided that the heart rate is unchanged
The stroke volume depends on preload, afterload as well as myocardial contractility. The preload is proportionate to the end-diastolic volume, while the afterload is the resistance against which blood is expelled (arterial blood pressure).
Factors affecting the cardiac output
- Venous return (preload).
- Efficacy of cardiac contractility.
- The arterial blood pressure (afterload).
- The heart rate.
- Blood volume and viscosity.
The End diastolic volume (venous return) (preload)
When the venous return is increased, the cardiac output will increase through the following mechanisms:
I- The relation between ventricular stroke volume and end-diastolic volume through the Frank-Starling curve. When an extra amount of blood flows into the ventricles, the cardiac muscle itself is stretched to a greater length. This in turn causes the muscle to contract with increased force. Therefore, the stroke volume is increased.
II- Stretch of the right atrial wall increases the heart rate by the atrial stretch receptor reflex; this, too, increases the cardiac output. Factors affecting the amount of blood returning to the heart likewise influence the degree of cardiac filling during diastole. Several mechanisms help to return the venous blood back to the right atrium:
1. The pressure gradient: The venous return is directly proportional to the pressure gradient between the right atrial pressure (RAP: the downstream pressure) and mean systemic filling pressure (PSF), The PSF depends on:
- Blood volume: There is a direct relationship between blood volume and Psf. The greater the blood volume, the higher the PSF, and vice versa.
- Venous compliance: There is an inverse relation between venous compliance and Psf. The more compliant the veins (can be stretched to compensate for larger volume), the lower the PSF and vice versa. Thus, constriction of the veins reduces the size of venous reservoirs, decreases venous pooling and increases venous return. In the supine position, the pressure gradient between Psf (about 7-10 mm Hg) and RAP (almost 0 mm Hg) tends to return the blood back to the heart. This factor disappears in a standing position due to the effect of gravity. However, the other factors help to maintain the pressure gradient and hence venous return in a standing position.
2. The skeletal muscle pump: The skeletal muscles are called the peripheral heart because they exert a muscle tone that compresses the veins and allows venous return. This is enhanced with muscular exercise due to increased muscle contraction.
3. The diameter of arterioles: arteriolar dilation increases venous return, while arteriolar constriction decreases venous return.
4. The capillary tone: Only 10% of the capillaries are opened under normal resting conditions. This maintains the venous return. However, if all the capillaries are opened at the same time, blood will accumulate in the capillaries and no venous return will occur (as in histamine shock).
5. The presence of valves in the veins: this prevents the blood from returning back & keeping it directed to the heart. (The valves are not present in the big, very small, and veins in the GIT and brain).
6. The inspiratory pump: Inspiration increases the intra-thoracic pressure negativity and the venous return.
7. Sympathetic stimulation causes constriction of the veins plus the other blood reservoirs (pulmonary veins, spleen & veins in the GIT).
All these factors increase the venous return, the end-diastolic volume, the stroke volume & the cardiac output.
Efficacy of myocardial contractility
Myocardial contractility is affected by the following factors:
- Neural input: When the sympathetic nerves to the heart are stimulated, the force of contraction increases. Circulating epinephrine and norepinephaugment the positive inotropic effect of norepinephrine liberated at the nerve endings. When the strength of contraction increases without an increase in fiber length, more of the blood that normally remains in the ventricles is expelled; that is the ejection fraction increases. Parasympathetic stimuli have the opposite effect.
- Ca2+ availability.
- The preload (Frank-Starling law).
- Changes in cardiac rate (HR) and rhythm: A high heart rate (pacemaker induced) produces a small increase in contractility (Bowditch effect). Because Ca2+ enters the cell more rapidly than it is sequestered by the sarcoplasmic reticulum, intracellular Ca2+ increases. However, increased heart rate to the extent that shortens the diastolic time will interfere with cardiac filling and cardiac contraction.
- Myocardial contractility is depressed in heart failure, hypoxia, and acidosis.
Starling mechanism & sympathetic stimulation increase myocardial contractility, but they do not use the same pathways. Sympathetic stimulation makes its effect by increasing the amount of Ca2+ entry from the extracellular fluid, thus increasing the intracellular calcium, while the Starling mechanism increases the sensitivity of the myocardial fiber to whatever Ca2+ may be there.
Afterload (arterial blood pressure)
Increased arterial blood pressure will interfere with the force of contraction. This causes an initial decrease in the stroke volume and cardiac output. Indeed, the end-diastolic volume of the next beat increases. This leads to increased force of contraction and stroke volume and cardiac output.
The heart rate
Heart Rate (HR): This refers to the number of heartbeats per minute. A higher heart rate increases CO, allowing the body to deliver more blood quickly in situations like exercise or stress.
Increased heart rate within limits increases cardiac output. The heart rate is primarily affected by autonomic nerves, with sympathetic stimulation increasing the rate and parasympathetic decreasing it.
Blood volume and blood viscosity
Increased blood volume helps the venous return, while hemorrhage decreases the venous return and cardiac output. On the other hand, increased blood viscosity retards the venous return, but in conditions of low blood viscosity such as anemia, the venous return and cardiac output are increased.
Factors Affecting Blood Pressure
Blood pressure is the force exerted by circulating blood against the walls of your arteries. It’s expressed as two values:
- Systolic pressure: The pressure when the heart contracts and pushes blood out.
- Diastolic pressure: The pressure when the heart relaxes and refills with blood.
Several factors can influence blood pressure
- Cardiac output: An increased cardiac output can elevate blood pressure if the peripheral resistance remains constant.
- Peripheral vascular resistance: The resistance to blood flow in the arteries. Constricted blood vessels increase resistance, raising blood pressure. Conversely, dilated blood vessels decrease resistance, lowering blood pressure.
- Blood volume: The amount of fluid in your circulatory system. Higher blood volume puts more pressure on artery walls, increasing blood pressure.
- Kidney function: The kidneys help regulate blood pressure by controlling blood volume and electrolyte balance. Impaired kidney function can contribute to high blood pressure.
- Age: Arteries tend to stiffen with age, leading to a rise in blood pressure.
- Diet: A diet high in sodium and low in potassium can contribute to high blood pressure.
- Lifestyle factors: Smoking, excessive alcohol consumption, stress, and lack of physical activity can increase blood pressure.
Maintaining a healthy lifestyle with regular exercise, a balanced diet, and stress management is crucial for optimal cardiovascular health and blood pressure control. If you have any concerns about your heart health or blood pressure, consult a healthcare professional.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download the application on Google Play from this link: Science Online Apps on Google Play
Mechanisms of cardiac reserve, cardiac work and oxygen consumption by the heart
Cardiac cycle importance, phases, diastole and systole, Aortic pulse curve and jugular venous
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart and Pericardium Structure, Abnormalities and Development of the Heart