Hepatocellular carcinoma symptoms, stages, risk factors, diagnosis and treatment
There are three main types of tumor: Benign, Premalignant, and Malignant, Benign is not cancerous, It does not invade nearby tissue or spread to other parts of the body, If a doctor removes them, they do not generally return, In premalignant, the cells are not yet cancerous, but they can potentially become malignant, Malignant tumors are cancerous, The cells can grow and spread to other parts of the body.
Malignant tumors
- Primary: HCC, Cholangiocarcinoma, Fibrolamellar carcinoma, and Angiosarcoma.
- Secondary.
Hepatocellular carcinoma (HCC)
HCC is the fifth most common cancer in the world, it occurs on top of known risk factors, (screening programs for detection of individuals who are more liable to develop).
Risk factors of HCC
- Cirrhosis is a precancerous condition whatever the cause e.g. steatocirrhosis, cryptogenic cirrhosis, and those patients need follow-up.
- Alcohol.
- Aflatoxin.
- Smoking, obesity, DM (recent risk factors).
Clinical picture
Early stages
- The patient may be asymptomatic (discovered accidentally during routine abdominal US we find a focal lesion on top of the cirrhotic liver.
- Or present with nonspecific manifestations (in patient known to be cirrhotic) as: fatigue, body ache, anorexia, weight loss even if mild, right hypochondrial pain, mild fever, malaise, loss of appetite.
Advanced Stages
Exaggeration of the already existing manifestation of cirrhosis as jaundice, ascites, variceal bleeding, and GIT bleeding, encephalopathy.
Rare presentations
Rupture (severe intra-abdominal pain and intra-abdominal bleeding and shock).
Paraneoplastic syndrome: variable manifestations present in patients with cancer regardless of the type of cancer far away from cancer and its site, and present with abnormal presentations like hypoglycemia, and hypocalcemia.
Investigations
Lab investigations are not conclusive in patients with HCC as we have a background of cirrhosis and disturbed liver profile:
1. Liver profile
- Enzymes: mild elevation or normal.
- Bilirubin: may be normal and usually increased (hepatocellular or obstructive).
- Tumor markers:
- There are no 100% conclusive markers to diagnose HCC.
- AFP (alpha-fetoprotein) most famous marker, if more than 200 ng/ml, but may not present as there are some types of HCC tumors that are not secretory tumors.
- Dysgamma carboxyprothrombin (DCP): which is also not conclusive for diagnosis of HCC.
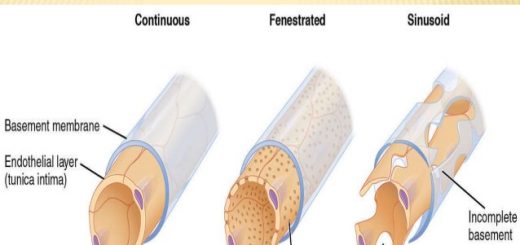
- VEGF (vascular endothelial growth factor).
2. Liver biopsy
- When imaging is NOT conclusive and the condition of the patient is suitable.
- We do liver biopsy whenever possible as most patients with HCC and cirrhosis are terminal patients and may have tense ascites and hyperbilirubinemia and defect in the coagulation profile so if the patient is not suitable wait until becomes able to this intervention.
3. Imaging
- Very important diagnostic tool than lab work.
- US: focal lesion in cirrhotic liver.
- US with contrast triphasic CT, and dynamic MRI.
- Triphasic CT shows a unique pattern: arterial enhancement and venous washout, so the tumor takes the contrast in the arterial phase and there is wash out of the contrast in the venous phase, so this finding by triphasic CT, dynamic MRI is conclusive for diagnosis of HCC.
To confirm diagnosis
- 2 dynamic imaging techniques (either contrast-enhanced MRI, triphasic CT and dynamic MRI) if mass 1-2 cm.
- Only 1 dynamic imaging technique if mass >2 cm.
- AFP>200 ng/ml but was removed from the guidelines as it is a deceiving tool for diagnosis as not all types of HCC are secretory. (BUT mention its name as it is a famous one).
For screening for HCC
- Abdominal US to detect focal hepatic lesions.
- Triphasic CT and/or dynamic MRI (according to size) for confirmation that is HCC, not another tumor related to the pathology of cirrhosis.
Staging of HCC
Many staging systems for HCC are present, but none of them are universally accepted, except for the Barcelona Clinic of Studying Liver Cancer (BCLC) staging system which is applied at Alexandria University. This staging takes into consideration: the clinical condition of the patient, performance status, size and number of lesions, and appropriate treatment for each stage (which is the most important issue in this staging system).
- In stages 0 and A: we can do resection (either segmentectomy or lobectomy), transplantation, or RFA.
- In stage B: either multi nodular more than 3 or single nodule more than 5 cm.
- In stage C: there is vascular invasion and we give either sorafenib or Nexavar.
- In stage D: we give only symptomatic treatment, for example:
- If the patient has ascites: adjust the dose of diuretics and do paracentesis to relieve the abdomen of the patient.
- If the patient has anemia: give multi-vitamins and a blood transfusion.
- If the patient has hypoalbuminemia: correct the albumin level.
- If the patient has hypoprothrombinemia: give a plasma transfusion. If he has abdominal pain due to the presence of a tumor: give analgesics.
Treatment strategies
1. Surgical resection
- Treatment of choice in very early stage, single tumor less than 2 cm and early stage (there are equal or less than 3 nodules each one is less than 3 cm or single nodule less than 5 cm.
- However, resection in patients with cirrhosis carries a risk of hepatic decompensation (due to decreased hepatic reserve) and the appearance of denovo lesions.
- Best outcomes (less risk for are associated with good selection criteria including: Good liver function, Good clinical condition: (well-compensated cirrhosis = Child A), and PHTN less than 10 mmHg.
2. Liver Transplantation
- We should stick to Milan criteria to achieve the maximum benefit of Liver Transplantation.
- Selection Criteria (Milan criteria) including:
- Solitary HCC < 5 cm or up to 3 nodules each < 3 cm.
- Absence of extrahepatic spread (vascular invasion = PV thrombosis or 2ry metastasis in the peritoneum or lymph nodes).
- These predictors give excellent outcomes after surgery with minimal risk for postoperative complication and liver failure (most important postoperative complication).
3. Local Ablation
This is the best therapeutic option for patients with very early and early stage HCC who are not suitable for resection or transplantation (due to location, co-morbidity, no donor, and cost). In this type of treatment destruction of the tumor cells is achieved by:
- Heating (Radiofrequency apparatus, Microwave, Laser).
- Injection of chemical substances Ethanol, Acetic acid, and Hot saline guided by a US needle or called electrode and injecting the chemical agents.
- Freezing (Cryotherapy).
Radio-frequency ablation (RF)
Advantages: Very effective ablation (curative therapy).
Disadvantages: Cost, bleeding, injury to vital structures such as blood vessels and biliary channels.
Technique:
- From outside we direct the tip of the needle or the electrode towards the center of the tumor guided by US.
- Rotate the handle of the needle and this rotation allows the release of certain arrays to get off the tip of the needle and lie in the center of the tumor, these arrays give the needle the shape of an umbrella so we have a wide surface area and can control the size of the surface area according to the size of arrays which appear from the tip of the needle.
- Now, the electrode or the needle is connected to the generator and heating and burning of the tumor tissue started.
- A similar electrode will allow freezing to get to the center of the tumor and kill the tumor cells by freezing in cryo apparatus or we can inject chemical substances which induce necrosis of malignant hepatocytes.
- This needle is like a classical needle but a little bit larger to go through the layers of the abdomen and parenchyma of the liver to reach the tumor.
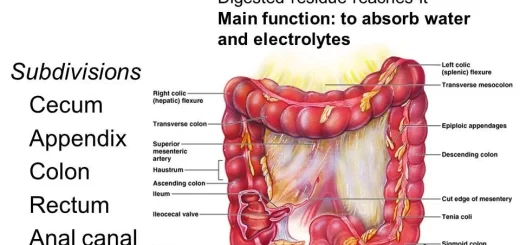
4. Trans-arterial chemo-embolization (TACE)
- Catheterization of the hepatic artery, then lobar and segmental branch which supplies the tumor directly to reach the center of the tumor.
- After this, the injection of a chemotherapeutic agent is followed by occlusion of the arterial flow by embolization to prevent the backflow of the chemotherapeutic agent, and by this, we close the feeding artery of the tumor so we kill the tumor by ischemia and chemotherapy and there is to harm to the surrounding liver parenchyma.
5. Sorafenib (Nexavar)
- Recent medication for the treatment of advanced stages of HCC.
- A multikinase inhibitor (acting on VEGF and PDGF receptor kinases), reduces tumor cell proliferation by inhibiting tumor angiogenesis, as every tumor secretes certain substances which induce angiogenesis (new blood vessel formation for this tumor), so stopping the renewal of blood supply of that tumor.
- This medication is not given in the early stages of HCC, given in advanced stages as its effect is not that marvelous and has multiple side effects.
- Side effects: thrombocytopenia, anemia, diarrhea, rash/desquamation, fatigue, abdominal pain, hand-foot skin reaction.
- So, patients taking this medication should be followed closely for developing one or more of these side effects to stop the medication or reduce the dose.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Hepatorenal syndrome (HRS) risk factors, diagnosis, symptoms, types, causes and treatment
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Liver Cirrhosis causes, symptoms, treatment & stages, Liver Biopsy and treatment of PHTN
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer
Common procedures of Interventional Radiology and the best Interventional Radiologists
Interventional radiology types, Robotic endovascular systems advantages & disadvantages