Carbon dioxide transport from tissues to lungs, Tidal CO2 and Haldane effect
CO₂ is not only a waste product of metabolism but it is also an important component of the carbonic/bicarbonate buffering system in the body fluids which is involved in the adjustment of pH. The solubility of CO₂ in the blood is about 20 times that of O₂; therefore, considerably more CO₂ than O₂ is present in simple solution at equal partial pressures.
Carbon dioxide transport
Carbon dioxide transport is transported in the blood in two forms:
1. Physically dissolved CO₂
About 5% of CO₂ is dissolved in the plasma and the RBCs. It is called free CO₂. It is very important because:-
- It is responsible for CO₂ tension (PCO₂) in the arterial blood (40 mm Hg) and the venous blood (46 mm Hg).
- It controls the direction and rate of flow of CO₂.
2. Chemically combined CO₂
It represents 95% of CO₂ content. It is present in two forms:
- Carbaminocompounds: About 5% is formed by the combination of CO₂ with the free amino group of plasma proteins and hemoglobin forming the carbamino compounds.
- Bicarbonate: It is the major form by which CO₂ is transported in the blood. About 90% of CO₂ content is present as bicarbonate ( KHCO3 in the RBCs and NaHCO3 in the plasma). The total CO₂ content in the arterial blood is 48 ml/100 ml and, in the venous blood, it is 52 ml/100 ml.
Tidal CO2
It is the volume of CO₂ that is added to each 100 ml of arterial blood during its flow through the tissues as a result of metabolism. It is normally about 4 ml 100m of blood at rest. It equals the difference between the total amount of CO₂ in the arterial and the venous blood (52- 48 = 4 ml).
Transport of CO2 from tissues to lungs (Chloride Shift)
A- Changes at the tissues
When blood is exposed to high CO₂ at the tissue, CO₂ passes from the tissues to the plasma. The following reactions take place:
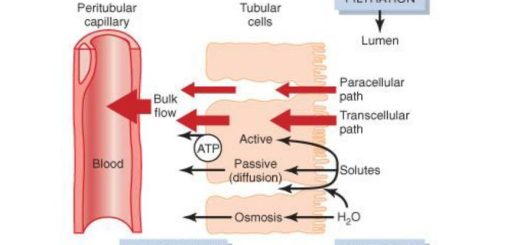
In plasma
- Small amount of CO₂ is hydrated forming carbonic acid which dissociates into hydrogen ions and bicarbonate (H+ and HCO3−). This reaction is very slow due to the absence of the carbonic anhydrase enzyme.
- Small amount of CO₂ combines with the amino group of plasma proteins forming a carbamino compound.
Inside RBCs
- Large amount of CO₂ diffuses from plasma to the RBC.
- CO₂ combines with H2O forming H2CO3 which dissociates to H+ and HCO3−. This reaction is accelerated 10,000 times by the enzyme carbonic anhydrase (C.A.) which is present in the RBCs. CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3−
- When the concentration of bicarbonate (HCO3−) inside RBCs increases, a greater part of it diffuses out of the RBCs to the plasma according to its concentration gradient.
- The chloride ions (CI−) enter the RBCs from the plasma to maintain the electrical neutralities. This movement of CI− is called the chloride shift. The CI− content in RBCs in venous blood is greater than that in arterial blood. For each CO₂ molecule added to a RBC, there is an increase of one osmotically active particle (CI−). Consequently, the RBCs take up water and increase in size. For this reason, plus the fact that a small amount of fluid in the arterial blood returns via the lymphatics rather than the veins, the hematocrit value of venous blood is normally 3% greater than that of the arterial blood.
- The H+ that is released after the dissociation of H2CO3 is buffered
- In the plasma by plasma proteins.
- In the RBCs by deoxygenated Hb which combines with H+.
Deoxygenated Hb is less acidic than oxygenated Hb and is a better H+ acceptor. The release of O2 from oxyheamoglobin into active tissues gives more reduced Hb which accepts more H+ (H+ + Hb ↔ HHb−). This allows more CO₂ transport by blood. HHb is a very weak acid that almost does not disturb the pH.
Small amount of CO₂ inside RBCs reacts directly with the amine radicle of Hb forming carbamino hemoglobin. This combination of CO₂ with Hb is a reversible reaction that occurs with a loose bond, so that CO₂ is easily released into the alveoli where the PCO2 is lower than in the tissue capillaries.
B- Changes at the lungs
At the lungs, the reverse processes to those of the tissues take place. When venous blood (PCO2 = 46 mm Hg) reaches the lungs, it is exposed to a lower PCO2 in the alveoli (PCO2 = 40 mm Hg). CO2 diffuses to the alveoli. The physically dissolved CO2 decreases and H+ binds to HCO3− → H2CO2 → CO2 + H2O. Accordingly, HCO3− concentration in the RBCs decreases therefore, HCO3 diffuses from the plasma to RBCs and Cl− diffuses to the plasma (chloride is shifted out of RBCs).
Haldane effect
It is the effect of oxygen-hemoglobin reaction on carbon dioxide transport. This effect is important in promoting carbon dioxide transport at the lung. The Haldane effect results from the simple fact that, the combination of oxygen with hemoglobin in the lungs causes the hemoglobin to become a stronger acid. This displaces carbon dioxide from the blood and into the alveoli in two ways:
- The more highly acidic hemoglobin has a less tendency to combine with carbon dioxide to form carbaminohemoglobin, thus displacing much of the carbon dioxide that is present in the carbamino form from the blood.
- The increased acidity of the hemoglobin also causes it to release an excess of hydrogen ions, and these bind with bicarbonate ions to form carbonic acid; this then dissociates into water and carbon dioxide, and the carbon dioxide is released from the blood into the alveoli.
Central and Chemical regulation of ventilation, Central and Peripheral chemoreceptors
Oxygen transport by blood, Importance of P50, Bohr Effect and Treatment of CO poisoning
Ventilation-perfusion relationships and why is ventilation higher at the base of the lung
Regional differences in ventilation, Pulmonary circulation, Shunt and Lung perfusion zones
Mechanics of ventilation, Structures of Respiratory system and Functions of conducting zone
Mechanics of Pulmonary Ventilation and Pressure changes during Respiratory cycle